Finger defect reconstruction using the radial artery superficial palmar branch free flap
Article information
Abstract
Purpose
The radial artery superficial palmar branch (RASP) free flap is accepted as a surgical technique for the reconstruction of finger defects. This study revisited the RASP free flap and evaluated its reliability and usefulness in a variety of finger defects.
Methods
From January 2017 to December 2022, multiple surgeons at a single institution performed a total of 315 RASP free flap reconstructions. Basic patient demographics and information on the finger defect and flap were assessed, and immediate postoperative flap and donor site-related complications were also studied. Data regarding long-term outcomes, such as the thumb joint range of motion and static two-point discrimination (S2PD), were collected and evaluated to identify statistically significant differences from the unaffected or non-innervated side.
Results
The mean postoperative follow-up was 14.8 months. The total flap survival rate was approximately 91.4%. There was no statistically significant difference in mean postoperative palmar abduction and radial abduction between the affected and unaffected thumbs in both groups. In the single-digit group, there was a statistically significant difference in S2PD between the innervated flap and unaffected side. A statistically significant difference was also found between innervated and non-innervated flaps in the multiple-digits group.
Conclusion
The RASP free flap is a valuable surgical option in reconstructing finger defects. It has already been proven to be safe and useful in coverage of single and tip defects. Stability should be ensured when there are multiple defects. Finally, the donor site morbidity is minimal and the recovery of sensation, once the flap is reinnervated, could be promising.
Introduction
Fingertip poses a great deal of functional importance. The sensory contact surface allows detailed proprioception, accurate two-point discrimination, touch, pain, and temperature sensation. For the last few decades, numerous attempts have been made to reconstruct the fingertip defect, including secondary healing, skin graft, local flap, distant flap, and free flap [1-17]. Reconstructing fingertip defects requires glabrous, durable, pain-free, and sensate tissue coverage. Reanimating aesthetically matching color and size is deemed of equal importance.
Traditionally, a thenar flap, in the form of a short-distance local flap, has been used for fingertip defect reconstruction [11,18,19]. However, concerns lay in the limited flap size, the possibility of joint contracture due to flexed posture for tension relief, and the potential need for skin grafting, leading to additional donor site morbidity. Moreover, when more than two fingertips need to be reconstructed simultaneously, the thenar flap is no longer an option.
Microsurgeons adopted free flaps to finger reconstruction to overcome the downsides of the local flaps. Free tissue transfer may have drawbacks, including long operating hours, the need for exquisite microsurgical skills, the risk of arterial insufficiency or venous congestion resulting in flap failure, and donor site morbidities. Nevertheless, when the surgery is performed desirably by a surgeon with sufficient microsurgical skills, the patient’s satisfaction with cosmetic and functional outcomes is unrivaled.
Furthermore, various free flap options are available, ranging from free thenar flap [19], hypothenar perforator free flap [20], digital artery perforator free flap [21], to free toe pulp flap [22]. If defect size goes beyond the fingertip, and especially if multiple fingers need to be reconstructed simultaneously, flaps of greater dimension, including posterior interosseous free flap [23], medial plantar free flap [24], and lateral arm free flap [25], should be considered.
Among these versatile surgical options, the radial artery superficial palmar branch (RASP) free flap is considered one of the most accepted reconstructive tools in the coverage of finger defects. Despite variations in the branching pattern of the RASP vessel [26-28], this flap is known for its many advantages. Besides providing a glabrous and color-matched tissue, it can also be sensate [2,29-33]. In addition, an operation can be done in a single field under a brachial plexus block without sacrificing a major artery. Furthermore, even though there may be variations in the pattern of RASP branching from the radial artery, skin perforators tend to arise consistently adjacent to the scaphoid tubercle [2,29-33]. The donor site, in most cases, can be primarily closed, and since thenar muscles are spared, thumb function is usually preserved [2,30,32]. Lastly, if harvested long enough, this flap can reconstruct multiple finger defects simultaneously.
Multiple surgeons in a single institution performed 315 RASP free flap reconstructions between January 2017 and December 2022. Fingers reconstructed were either single or multiple, ranging from two to four. Previously, many studies have been published to evaluate the usefulness and safety of this particular flap [2,29-33]. In this paper, the authors revisited the RASP free flap. We tried to elaborate on its reliability in finger defect reconstruction by retrospectively reviewing the clinical outcomes of a few hundred subjects.
Methods
Ethics statement: This study was performed in accordance with the Declaration of Helsinki and received approval from the Public Institutional Review Board Designated by Ministry of Health and Welfare (No. P01-202305-01-014). Written informed consent was obtained from the patient for the publication of this report including all clinical images.
We conducted a retrospective review of the patients who received a RASP free flap reconstruction between January 2017 and December 2022 in a single institution by multiple surgeons. A total of 315 patients were included in the study. The mean age of the patients was 47.8 years old (range, 21–73 years), and there were 286 males and 29 females. The vast majority, 302 patients, underwent a reconstruction due to immediate industrial trauma. Nine patients’ injury mechanisms lied in residential settings, such as car door crush amputation and human or animal bite amputation. Four patients underwent reconstruction to alleviate the tip pain associated with soft tissue atrophy from the old injury.
The patients were divided into two groups: 278 single digit and 37 multiple digits involvement. Defect and flap demographics are outlined in Table 1. Right and left hand involvement accounted for 136 and 179 patients, respectively. The injured digits among single digit involvement were 41 thumbs, 88 index fingers, 81 long fingers, 37 ring fingers, and 31 little fingers. By specific location, volar side involvement summed up to 244 cases, and the remaining 34 patients had both volar and dorsal sides involved. Meanwhile, of the 37 patients with multiple digits involvement, six patients had three or more fingers involved simultaneously. Eleven cases involved only the volar side, whereas 26 patients needed the volar and dorsal side to be reconstructed. No patients had bilateral hands involvement.
Flap and donor site complications were monitored immediately after the operation. Partial or total flap necrosis, arterial insufficiency, venous congestion, need for revision or salvage procedure, wound problems, and need for additional debridement or other reconstructive procedure were all evaluated. The mean postoperative follow-up was 14.8 months (range, 2–48 months). Long-term complications, for instance, epidermal cyst, neuroma, tip pain, and scar contracture, were also evaluated. At 12 months postoperatively, the thumb joint range of motion was compared with the unaffected side. Finally, the donor site scar was inspected for hypertrophic change or keloid contracture. Static two-point discrimination (S2PD) with the two-point discriminator (Fabrication Enterprises, Inc., Elmsford, NY, USA) was used to assess the sensibility of the flap in comparison to the unaffected finger or non-innervated flap.
1. Statistical analysis
All statistical analyses were performed using IBM SPSS Statistics ver. 25 (IBM Corp., Armonk, NY, USA). Continuous variables were calculated as the mean and range or standard deviation, as appropriate. Categorical data were expressed as a frequency (proportion, %). The paired t-test was used to evaluate whether there was a statistically significant difference in the means of the continuous variables between the two groups—mean postoperative palmar abduction and radial abduction and S2PD. A p-value of <0.05 was considered statistically significant.
2. Surgical strategy
Important landmarks in elevating the RASP free flap were the scaphoid tubercle, radial artery, flexor carpi radialis, and palmaris longus tendons (Fig. 1A, 1C). Before the actual surgery, the scaphoid tubercle was digitally palpated, and the portable mini-doppler was used to confirm the presence of a direct skin perforator. A color Doppler ultrasonography was also done to identify the origin of the RASP vessel (Fig. 1B).
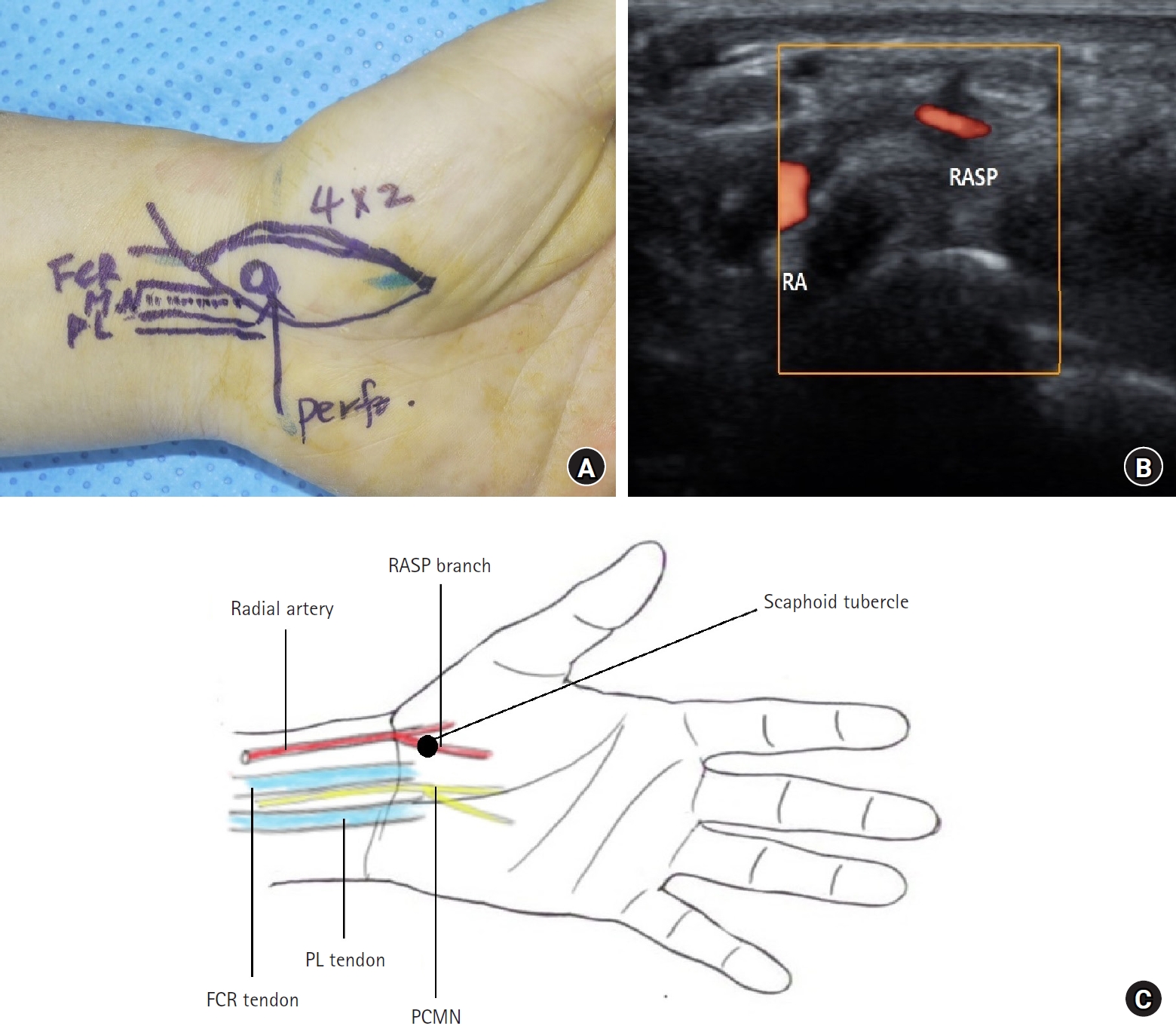
(A) Important surface landmarks in elevating the radial artery superficial palmar branch (RASP) free flap. (B) Preoperative color Doppler ultrasonography to identify the origin of the RASP vessel. (C) Schematic diagram of the anatomical landmarks in elevating the RASP free flap. FCR, flexor carpi radialis tendon; MN, median nerve; PL, palmaris longus tendon; Perf., direct skin perforator nearby scaphoid tubercle; RA, radial artery; PL, palmaris longus; PCMN, palmar cutaneous branch of the median nerve.
Under the supine position, all 315 patients received surgery under ultrasound-guided brachial plexus nerve block. Pneumatic tourniquet compression was used throughout the surgery. First, the finger defect was debrided and examined under a microscope to locate the recipient artery, veins, and nerve. If multiple digits were to be reconstructed, surgeons had to decide which finger to use as a recipient for arterial anastomosis and whether to use other fingers for additional venous drainage.
After measuring the defect size, the flap, slightly larger than the defect, was marked on the patient’s skin. Harvesting the flap with a dimension greater than the defect was essential due to progressive skin contracture and volume decrease. In cases of multiple-digit reconstruction, for adequate soft tissue coverage during subsequent flap division, the flap was inset with web spaces in a more abducted position (Fig. 2A). Extra flap length was required in the multiple-digit reconstructions. When three or more digits were involved, the flap length required usually exceeded 10 cm (Fig. 2B). In most cases, the flap was designed in an elliptical fashion with the scaphoid tubercle located at the proximal center. However, since defects came in various shapes, surgeons elevated flaps of other designs, including reverse T-shaped flaps (Fig. 2C).

(A) Flap inset during the reconstruction of multiple digits. Adequate web-space abduction when measuring the flap length and insetting the flap. (B) Large flap with length exceeding 10 cm for reconstructing three or more fingers. (C) Reverse T-shaped radial artery superficial palmar branch free flap
Flap was elevated starting from the proximal radial ends, progressing into the distal ulnar direction. At first, it was of utmost importance to find the RASP branching from the radial artery (Fig. 3A). Surgeons should always anticipate the variations in the branching pattern of the RASP when dissecting the vascular pedicle. Both vena comitantes and dermal veins at the proximal end of the flap were harvested for later anastomosis. As the caliber of the dermal vein was presumed to be inversely proportional to that of vena comitantes, if a large dermal vein was noted, surgeons harvested the dermal vein within the flap. In some instances of multiple-digit reconstruction, the dermal vein at the distal end of the flap was also saved for extra venous drainage.
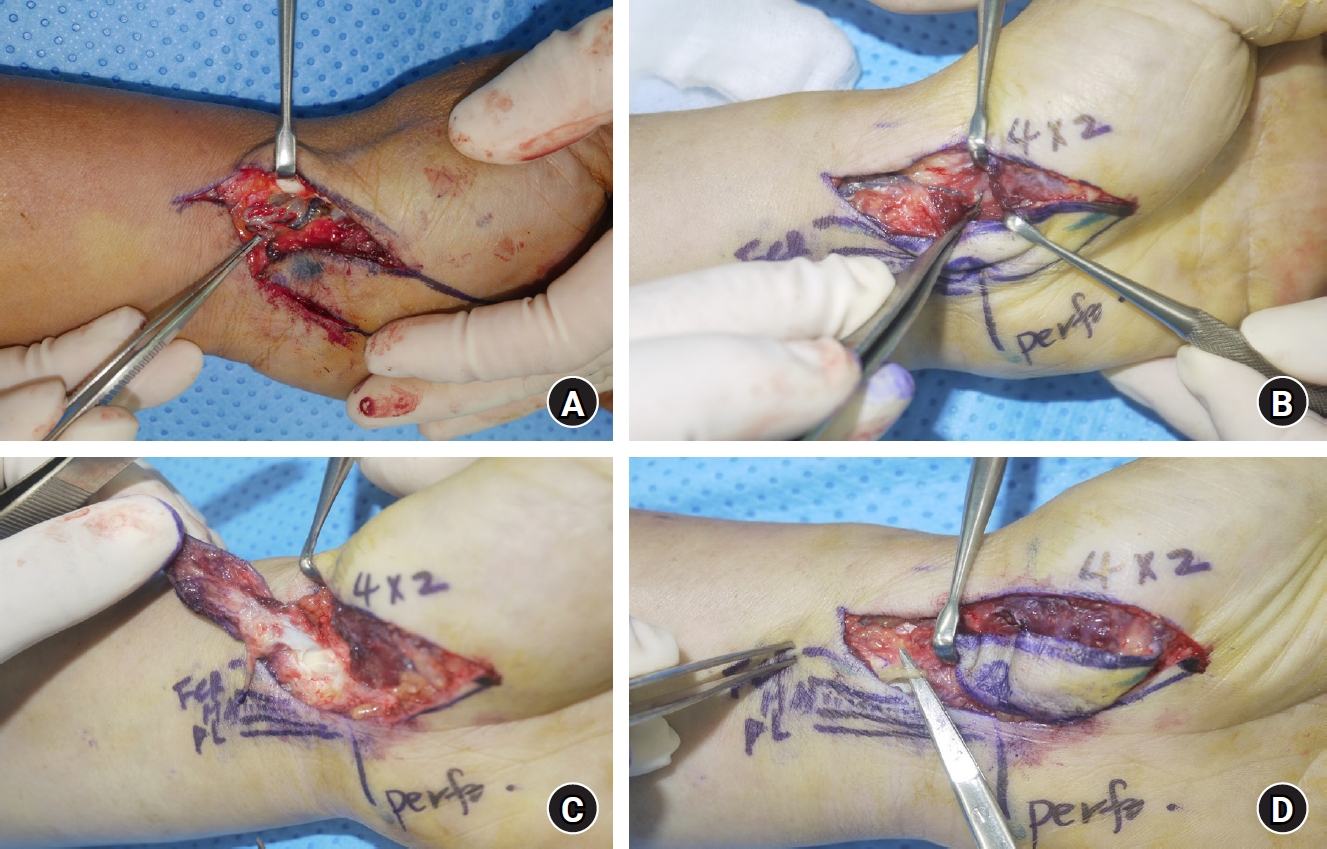
(A) Radial artery superficial palmar branch (RASP) arising from the radial artery and its venae comitantes. (B) Ligation of the efferent ends of the RASP branch and vena comitans. (C) Harvest of the flexor carpi radialis tendon sheath with the flap. (D) Harvest of the palmar cutaneous branch of the median nerve with the flap. Perf., direct skin perforator nearby scaphoid tubercle; FCR, flexor carpi radialis tendon; MN, median nerve; PL, palmaris longus tendon.
Flap was elevated above the superficial palmar fascia, sparing the thenar muscles. Efferent ends of the RASP branch and vena comitantes were ligated (Fig. 3B). Proximal to the scaphoid tubercle, a portion of the flexor carpi radials tendon sheath was included within the flap for easier, faster, and safer dissection (Fig. 3C). If present, a palmar cutaneous branch of the median nerve (PCMN) was harvested with the flap for sensory reinnervation (Fig. 3D).
After positioning the harvested flap over the defect, the flap artery was initially anastomosed to the digital artery, and either one, two, or even three vein anastomoses were followed. If PCMN was included in the flap, neurorrhaphy was also done. Flap’s proximal end was inset in a VY fashion to prevent venous occlusion. Most radial or ulnar-sided finger artery was used for arterial anastomosis in the multiple-digit reconstruction. A subcutaneous vein on the same finger was usually anastomosed to the flap vein. Suppose the flap length exceeded 10 cm, and venous drainage at the distal end of the flap was concerned. In that case, surgeons should perform another vein anastomosis between the dermal vein at the distal end of the flap and the subcutaneous vein in the finger other than the recipient. If the vascular pedicle was exposed, immediate skin grafting over the pedicle was considered.
The donor site was closed primarily in most cases. If the flap was inset into multiple digits, the flap division procedure was followed 2 or 3 weeks after the initial surgery. When three or more fingers were in reconstruction, at least two division procedures were required with 2 to 3 weeks of revascularization period in between. When dividing the flap, z-plasty was used for adequate soft tissue coverage (Fig. 4).

Preoperative and postoperative views of z-plasty for flap division in the reconstruction of multiple digits. Note the red lines for z-plasty incision.
Once the flap circulation stabilized, a postoperative rehabilitation procedure was initiated, generally one week after the surgery. Both passive and active joint motion were exercised by gradually increasing the degree as the patient’s pain subsided. If partial necrosis or wound dehiscence was suspected, an additional debridement procedure was done 3 weeks postoperatively. The debulking procedure, if necessary, was performed at least 6 months postoperatively.
Results
Of the 315 patients, 278 patients had a single-digit reconstruction. Their clinical outcomes were analyzed separately from those with multiple digits involvement. As outlined in Table 1, the mean dimension of the defect was 2.1×3.9 cm2 (range, 1.5×5.0 cm2 to 2.0×8.0 cm2), and that of the flap was 2.3×4.9 cm2 (range, 1.5×5.0 cm2 to 2.0×9.0 cm2). On the other hand, the mean dimension of the flap, required for defect coverage in the multiple-digit reconstructions, was 2.1×6.4 cm2 (range, 1.8×3.5 cm2 to 3.0×12.0 cm2). Defect measurement data was not included in the multiple-digit reconstruction group.
Microanastomosis results are also shown in Table 1. Within a single-digit reconstruction group, an ulnar and radial digital artery was used as a recipient vessel in 189 and 89 cases, respectively. In contrast, 19 and 18 the multiple-digit reconstruction group cases used ulnar and radial digital arteries, respectively. In the single-digit group, 184 (out of 278) patients had one vein anastomosis; 94 patients had two or more veins anastomosed; however, two had three veins anastomosed. When reconstructing the multiple digits, the number of two vein anastomoses exceeded that of the single anastomosis by 29 to eight cases. RASP branch or perforator rarely perfused blood into the flap, and surgeons had to convert the flap into a venous free flap by connecting the recipient artery to the flap’s dermal vein. Seven such cases were in a single-digit reconstruction, whereas none was found in the multiple-digit reconstruction group.
As highlighted in Table 2, the flap survival rate was approximately 91.4% (288 out of 315). Of the 22 flap necrosis cases, eight partial and 14 total, in a single-digit reconstruction, five patients’ wounds healed by secondary intention only. Additional skin grafting or other flap surgeries, such as cross-finger or groin flap, were done in four cases each. Nine patients who refused further reconstructive procedures underwent complete removal of the necrotic flap and stump revision. The above numbers were as follows in the multiple-digit reconstruction group: secondary healing, 3; skin grafting, 1; other flaps, 0; and amputation and stump revision, 1.
Flap failure was attributed to arterial insufficiency or venous congestion. When arterial insufficiency was noted, surgeons examined the microanastomosis site again on the operation table. Fourteen out of 278 single-digit reconstruction cases required a simple artery reanastomosis. Three patients needed another digital artery for supercharging to the flap’s dermal vein. Two patients used a vein graft to relieve the pedicle tension. No arterial sufficiency was noted in the multiple-digit reconstruction group.
Venous congestion was a more frequently observed flap circulation problem. Among 25 venous congestion cases in the single-digit reconstruction, simple vein reanastomosis was done in 10 cases, while the flap congestion subsided by salvage procedure using medical leeches in seven patients. Multiple-digit reconstruction with a much longer flap might have a higher risk of venous congestion, especially at the distal end. Fortunately, only one case was reported to have postoperative venous congestion, which was resolved by applying medical leeches for a few days.
Three weeks after the initial flap operations, surgeons debrided the flap if partial wound necrosis or dehiscence was concerned. These cases summed up to 28 and six cases in the single and multiple-digit reconstructions, respectively. Flap debulking was delayed at least 6 months postoperatively. Nine patients with a single-digit reconstruction had a part of the flap debulked, mainly for cosmetic purposes. No multiple-digit reconstruction patient wanted a debulking procedure.
Long-term complications ranged from an epidermal cyst, neuroma causing pain and paresthesia, and tip pain to scar contracture. Eight patients in a single-digit reconstruction group had epidermal cysts or neuromas removed (four each). Six patients suffering from tip pain had their bone tips excised. Two patients with scar contracture received a z-plasty for tension relief. Neuroma and tip pain were noted in two patients each in the multiple-digit reconstruction.
Donor site demographics and morbidities are described in Table 3. In most cases, the donor site was primarily closed; delayed primary closure had to be done 3 weeks postoperatively in three cases. Two patients in each group complained of hypertrophic scar or keloid at the donor site. However, no additional surgery or injection was necessary. Symptomatic neuroma might be a concern at the distal end of the resected nerve at the donor site, yet no case was found in the study. The thumb’s mean palmar and radial abduction were measured to estimate the preserved thumb function at the elevated flap side in certain cases, 18 and 12 cases of the single and multiple-digit reconstructions. In the single-digit reconstruction group, the mean values of thumb on the affected side were 58.6°±5.09° and 58.9°±5.57°, while those on the unaffected side were 59.2°±6.47° and 59.7°±5.55°. No statistical significance was proven as the p-values were >0.05. Likewise, in the multiple-digit reconstruction group, there was no statistically significant difference in the thumb’s range of motion between the flap harvested and unaffected sides. Mean values were 56.7°±4.92° and 59.2°±4.17° at the affected thumb, and they were 58.8°±5.28° and 60.8°±4.69° at the unaffected thumb.
Nerve coaptation of the flap was accomplished by harvesting PCMN with the flap. Table 4 summarizes the clinical outcomes of nerve coaptation. Harvested nerve was microanastomosed to the recipient digital nerve in 135 and 17 cases of the single- and multiple-digit reconstructions, respectively. At 12 weeks postoperatively, S2PD was measured in 20 and 11 single- and multiple-digit reconstruction group patients. S2PD was measured at the reconstructed and unaffected fingers in the single-digit reconstruction group. On the other hand, in the multiple-digit reconstruction group, S2PD was measured at the innervated and non-innervated flap.
The mean S2PD of the innervated finger in the single-digit group was 7.6±2.39 mm, and that of the unaffected finger was 4.05±1.36 mm. The difference was statistically significant (p<0.05), implying despite nerve innervation, the two-point discrimination ability of the reconstructed finger varied from that of the unaffected finger. In the multiple-digit reconstruction group, the mean S2PD of the innervated flap differed from that of the non-innervated flap by 9.64±3.23 to 14.2±0.98 mm. A statistically significant difference was proven, as the p-value was 0.001. Nerve reinnervated flap in the patients with multiple-digit reconstruction might have gained a certain degree of sensation recovery compared with those without nerve reinnervation.
1. Cases
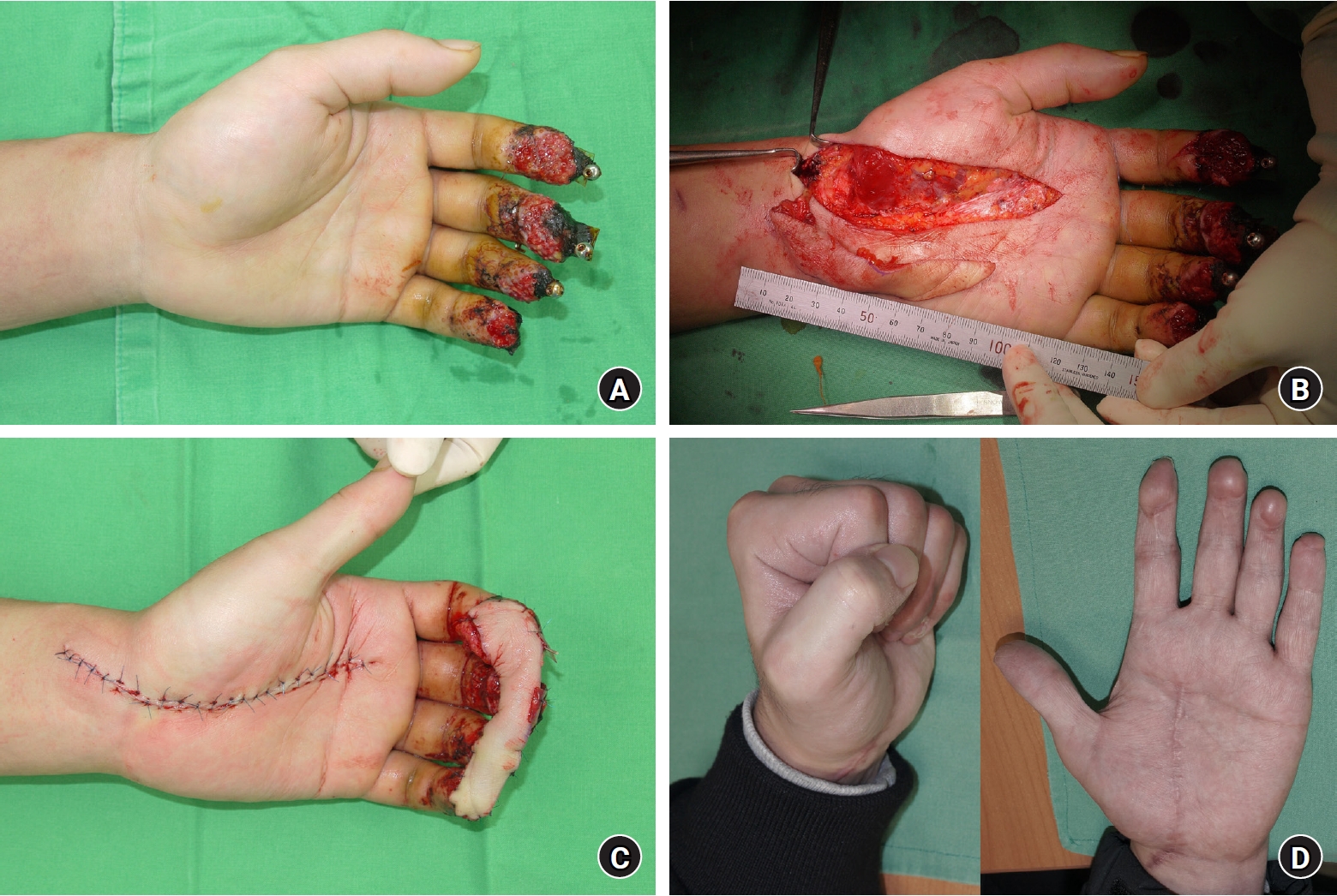
Case 1. Large radial artery superficial palmar branch flap reconstruction for four fingertips reconstruction
A 25-year-old male was admitted for traumatic crushing amputations of the left index, long, ring, and little fingertips due to hydraulic machine injury (Fig. 5A). After initial bone fixations and 3 weeks of secondary healing, RASP free flap with dimension of 2.0×12.0 cm was harvested (Fig. 5B) and inset into soft tissue defect, and donor site was closed primarily (Fig. 5C). Flap survived without any postoperative venous congestion or necrosis. Throughout the sequential flap division procedures with z-plasty, all four fingertips were reconstructed. One year postoperatively, the patient exhibited a near-full range of motion of all joints without any long-term complications (Fig. 5D).
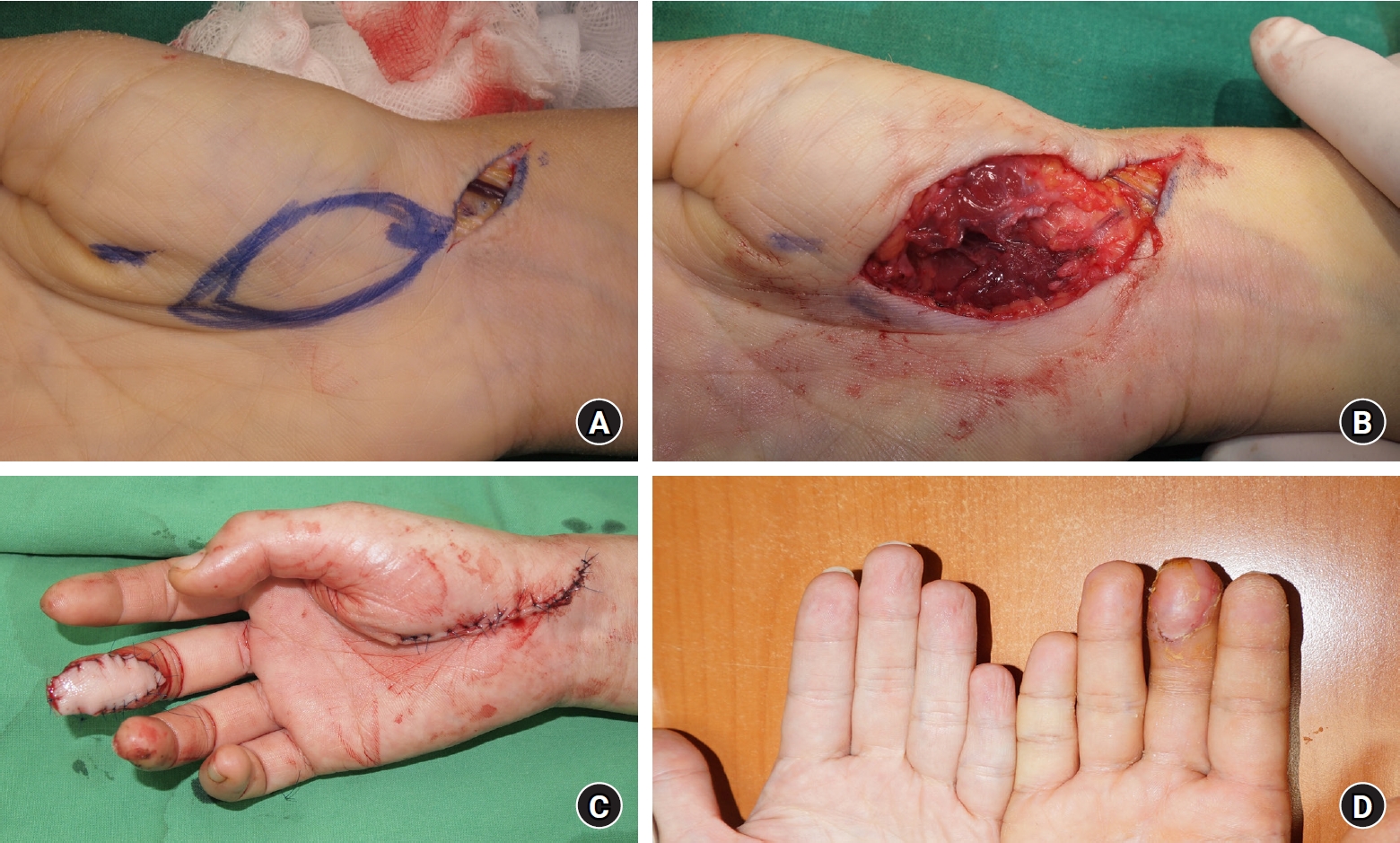
Case 2. Reverse T-shaped radial artery superficial palmar branch flap reconstruction for two fingertips reconstruction
A 37-years-old male visited the emergency room for left long and ring fingertips soft tissue amputation caused by machine belt injury (Fig. 6A). Size of the defects of the two fingers varied and the ring finger defect involved not only the volar side but also the dorsal side. Conventional elliptical-shaped flap might not fully cover the defect. Therefore, a 2.0×7.0+2.0×5.0-cm sized reverse T-shaped flap was elevated (Fig. 6B). Flap was inset into the defect (Fig. 6C), and 3 weeks after, flap division was performed. Flap survived without any complications. One year postoperatively, the patient displayed a near-full range of motion in the affected digits, and no long-term complications were noted (Fig. 6D).

(A) Left long and ring finger traumatic crushing amputations with a ring finger defect involving both the volar and dorsal sides. (B) Harvest of 2.0×7.0-cm and 2.0×5.0-cm reverse T-shaped radial artery superficial palmar branch flaps. (C) Inset of the flaps into the defect. (D) One year postoperative.
Case 3. Radial artery superficial palmar branch free flap with sequential iliac bone strut graft
A 49-year-old male had a traumatic ripsaw injury on his left index, long and ring fingers. While long and ring fingers only required a bone fixation and repair of tendon, artery, and nerve, the index finger had both soft tissue and distal phalanx bone defect (Fig. 7A). Initially, soft tissue reconstruction was done using a 2.0×4.0-cm sized RASP free flap (Fig. 7B). Once the flap stabilized without any postoperative complications, bone defect reconstruction was planned. Autogenous iliac bone strut graft was harvested and fixated into the defect by means of joint arthrodesis (Fig. 7C). One year postoperatively, although the distal interphalangeal joint was no longer mobile, sufficient bone length was acquired, meeting the patient’s satisfaction and limiting dead space between the soft tissue and bone tip (Fig. 7D).
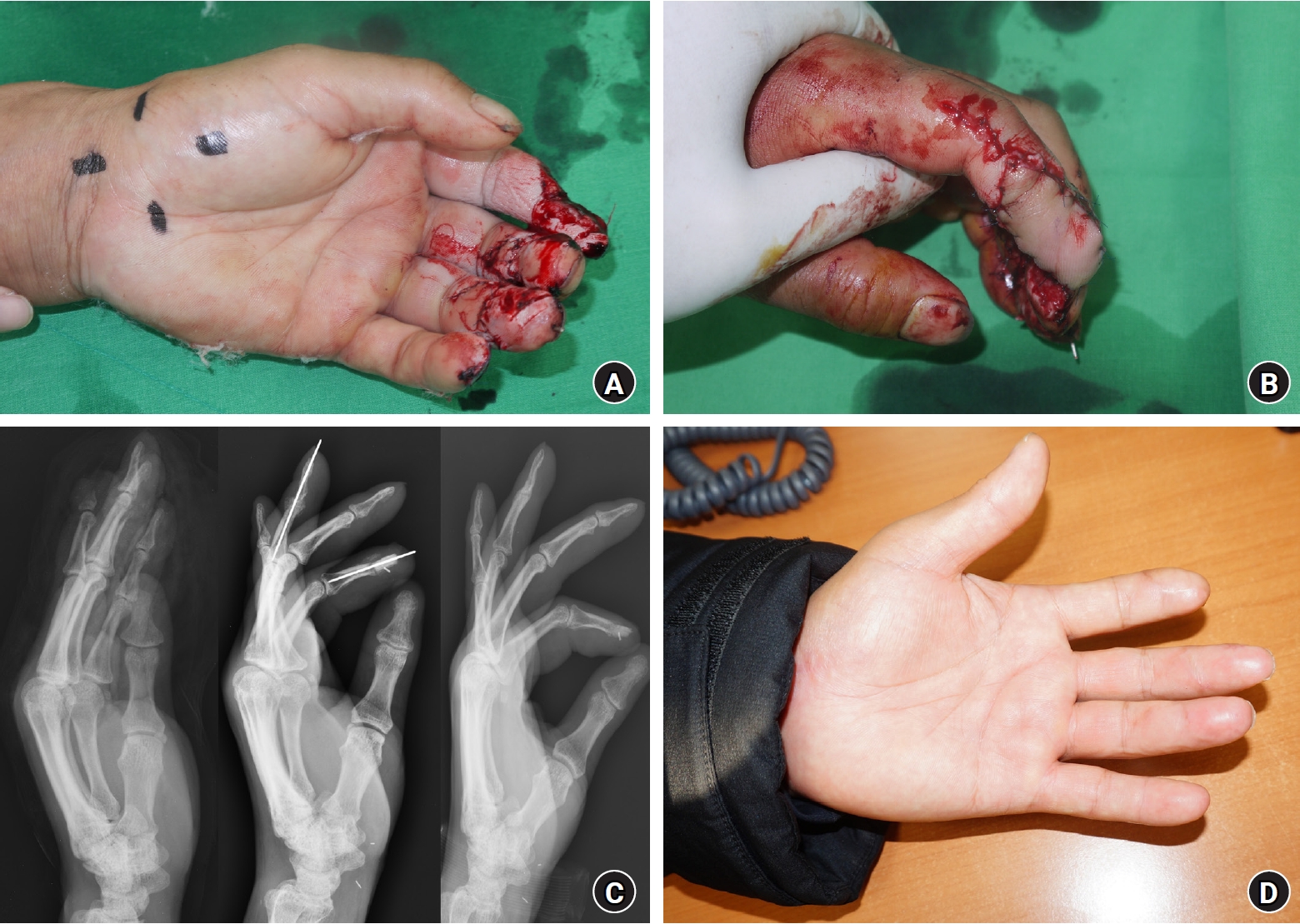
(A) Left index finger soft tissue and bone defect. (B) A 2.0×4.0-cm radial artery superficial palmar branch free flap for soft tissue reconstruction. (C) Preoperative, immediate postoperative, and 1-year postoperative views of the iliac bone strut graft on the distal phalanx bone defect. (D) One year postoperative.
Case 4. Venous free flap conversion of the radial artery superficial palmar branch flap
A 26-year-old female had a right long fingertip traumatic amputation from the roller machine injury. Approximately 2.0×3.0-cm sized defect was in need of reconstruction. In a usual manner, RASP free flap reconstruction was planned. At the proximal end of the flap margin, a large-sized dermal vein was noted and saved just in case (Fig. 8A). During the flap dissection, the vascular pedicle was accidentally damaged (Fig. 8B). Therefore, a surgical plan had been changed to converting the flap into venous free flap using the previously saved dermal vein for microanastomosis with the recipient digital artery (Fig. 8C). Medical leeches were used immediately after the surgery for 5 days for prevention of venous congestion. Fortunately, the flap survived without necrosis from venous congestion throughout the entire admission period. One year postoperatively, the patient complained of no long-term complications (Fig. 8D).
(A) Dermal vein at the proximal end of the radial artery superficial palmar branch (RASP) flap. (B) Elevation of the RASP flap with the vascular pedicled damaged accidentally during flap dissection. (C) Conversion of the RASP free flap into a venous free flap and inset of the flap into the defect. (D) One year postoperative.
Discussion
Multiple factors need to be considered when reconstructing a finger defect. Defects range from a mere soft tissue to the nailbed complex, nerves, bone, and joints. Therefore, besides the patient’s age, gender, underlying comorbidities, and general conditions, the size and degree of the soft tissue defect and the need for sensate and/or osseous recovery affect which type of reconstruction tool to be selected [12]. Reconstructing the fingertip requires a durable and glabrous tissue recovery. In particular, pulp tissue at the tip of the finger needs to remain pain-free and sensate simultaneously. In this sense, aesthetic and functional recoveries are equally important in fingertip defect reconstruction.
Conservative management may be sufficient for a simple, minimal defect by waiting for a secondary intention to heal, primary closure, or skin grafting [5-9]. Various local flaps are available for more in-depth injuries [1,3-6,9,10,13,14]. However, if multiple fingers are affected or the size of the defect is large, the local flap alone may be restrictive.
Despite their drawbacks, local flaps are still widely used. Namely, the thenar flap and cross-finger flap are useful, as they provide the tissue with similar characteristics to the defect [15,16]. Nevertheless, more than two surgeries are generally required. Joint contracture, limited flap size, additional donor site morbidity, and inability to re-innervate the defect and reconstruct multiple fingers are still issues to be addressed. Various free flaps have been introduced as an alternative [17,19-25]. Once the surgeon gets well-acquainted with the microsurgical skills, free tissue transfer can promise outstanding results in both aesthetic and functional aspects.
The RASP free flap is notably one of the most frequently used free flaps, which is also true in the author’s institution. One of the key elements in selecting the flap type is the surgeon’s preference, as flap survival is closely linked to the surgeon’s familiarity with the flap. This can improve surgical outcomes by shortening operating hours, elevating the flap more safely and easily, and facilitating postoperative patient care. In this study, authors presented the clinical outcomes of 315 patients whose finger defects were reconstructed using a RASP free flap during the last 6 years.
The thenar region has been commonly selected as a donor site for various free flaps. These flaps have historically evolved from one to another, beginning from the free thenar flap to the free radial thenar flap, a free superficial palmar branch of the radial artery flap, and a free innervated RASP branch flap [2,11,18,19]. Some share similar nomenclature, and all have RASP as a donor artery.
The RASP free flap can serve many purposes. Just like other free flaps, it provides durable and glabrous tissue. Moreover, it affords a tissue that matches the color and size of the finger and fingertip defects. Unlike local flaps, it can cover soft tissue defects of a substantial size. Furthermore, as it can be harvested as long as 10.0 cm or even longer, it can reconstruct multiple fingertip defects simultaneously [33,34]. As exemplified in case 1, 37 patients had multiple fingertip defects, as many as four, reconstructed using a single RASP free flap in this study. A survival rate of 86.5% proved the stability of this flap for multiple finger defect reconstruction.
The elliptical flap is a standard choice of shape in the RASP flap. However, fingertip defects do not always come in a desirable shape. Just as surgeons can extend the flap length over 10.0 cm, they can also change the flap shape to suit the purpose. As in case 2, surgeons managed to elevate the flap of a reverse T-shape, which adequately fit the defect. At the same time, there was no need for extra skin grafting or delayed closure for the donor site.
Due to its inability to supply osseous support, the RASP free flap has limited use in finger defects that require bone reconstruction. In case 3, the patient’s fingertip defect involved the soft tissue and bone structure. A RASP free flap cannot provide osseous reconstruction to the defect; however, once stabilized, it can offer a tolerable soft tissue environment for establishing the bone graft of another origin to the recipient.
From the surgeon’s perspective, surgery can be done in a single operative field under a brachial plexus block without concerns about the side effects of general anesthesia. There may be variations in the pattern of RASP branching from the radial artery; however, the throbbing of the direct skin perforators is observed in an anatomically similar pattern [2,29-33], facilitating the flap dissection steps. In addition, as shown in case 4, even if the vascular pedicle is accidentally damaged, there is still a chance of salvaging the flap by converting it into a venous free flap, as a dermal vein with a large-sized caliber is readily available nearby the flap margins.
The free thenar flap and free radial thenar flap reconstruct an innervated tissue coverage with a superficial sensory branch of the radial nerve or lateral antebrachial cutaneous nerve [2,19,29]; however, the RASP free flap re-innervates the defect with PCMN, which usually is anatomically consistent and fits the size of the digital nerve [2,29]. Furthermore, previous studies suggested a possibility of sensate recovery in the finger defect reconstructed with an innervated flap [15,34-37]. Likewise, this study revealed that among patients with multiple-digit reconstructions, fingers with the reinnervated flap displayed a statistically significant difference in mean S2PD compared with fingers with the non-innervated flap. On the other hand, among the patients with only one finger reconstruction, the mean S2PD of the affected finger could recover to the level of the unaffected finger. The study’s findings, however, lack reliability and validity, as only 20 and 11 out of 135 and 17 of the single-digit and multiple-digit reconstruction groups, respectively, were included for statistical analyses.
The donor site of the RASP flap is closed primarily without difficulty [29-33]. In this study, primary closure was possible 99.0% of the time. Three patients whose donor site could not be primarily closed did not undergo any additional skin grafting but waited 3 weeks for delayed primary closure. Despite successful defect reconstruction, patients may complain of scarring at the donor site a few months later at the outpatient clinic. Fortunately, the authors encountered only two patients who developed hypertrophic scar or keloid at the donor site, and no dissatisfaction was noted. In addition, since thenar muscles are spared when elevating the flap, the thumb function is usually preserved [29-33]. To evaluate such morbidity, the authors also compared mean postoperative palmar abduction and radial abduction of the affected thumb to that of the unaffected. There was no statistically significant difference in both single-digit and multiple-digit groups. Even after a portion of the soft tissue was removed from the thenar region, the thumb joint function was similar to that of the normal side. Nevertheless, the limited sample size compromised the reliability of this suggestion.
This study has a strength in its large study subjects and substantially long follow-up periods. Clinical outcomes of a few hundred patients were detailed and presented as objective data. Furthermore, all data were collected only in one institution, dismissing the potential confounding variables in different centers. Nevertheless, due to the retrospective nature, the clinical outcomes’ validity and reliability might be questionable relative to the prospective studies. Furthermore, only two were evaluated for statistical significance among numerous continuous variables studied. The number of subjects included for statistical analysis accounted for only one-tenth of the subjects. Including another data set to assess the sensory outcome, including Semmes-Weinstein monofilament and moving two-point discrimination, could have added reliability to the study. Lastly, the study was conducted only from the perspective of the surgeons. Perhaps, patients’ actual satisfaction measured in a visual analog scale for pain assessment or a questionnaire for specific dissatisfaction could enrich the depth of the study.
Conclusion
RASP free flap is a valuable surgical option in reconstructing the finger defect. It has already been proven to be safe and useful in coverage of the single and tip defect. Stability should be assured when defects are multiple, as well. Finally, donor site morbidity could be minimal and recovery of the sensation, once the flap is reinnervated, could be promising.
Notes
The authors have nothing to disclose.
Funding
None.