흉배동맥 천공지 유리 피판술을 이용한 광범위 수부 손상의 재건: 2예의 증례 보고
Reconstruction of a Mangled Hand with a Thoracodorsal Artery Perforator Free Flap: A Report of Two Cases
Article information
Trans Abstract
Mangled hands are a severely injured condition that is a rare and challenging problem for reconstructive surgeons. Surgical flaps such as anterolateral thigh, radial forearm, or thoracodorsal artery flaps have been used for multiple-digit resurfacing. In this report, we describe two cases of complex defects that included multiple digits in patients who underwent reconstruction with thoracodorsal artery perforator (TDAP) free flaps. All massive soft tissue defects were completely covered with a TDAP free flap. The thinner perforator flap could be harvested, and the patients regained the ability to pinch and grasp. Therefore, the authors present two cases of mangled hands successfully treated with TDAP free flap.
INTRODUCTION
Mangling hand injuries are a rare and challenging problem for reconstructive surgeons. In such cases, surgeons should consider soft tissue reconstruction with early functional recovery. Numerous free flaps are available for the reconstruction of hand defects, including radial forearm, anterolateral thigh (ALT), thoracodorsal artery perforator (TDAP), and circumflex scapular artery perforator flaps. Recently, perforator free flaps have been commonly used for hand reconstruction because of their versatility, thinness, and minimal donor site morbidity [1,2]. The authors thought that the TDAP free flap can be the most suitable flap for reconstructing complex hand injuries because its thinness enables patients to retain their earlier ability to pinch and grasp and the donor site on the back is less exposed than that on the extremity [3].
Herein, we report two cases of mangled hand after a press machinery injury treated with a TDAP free flap in two patients. We discuss the results with a literature review.
CASE REPORTS
1. Case 1
A 46-year-old man had a crushing injury involving the thumb and index, middle, and ring fingers of his dominant, right hand due to a power press machine accident. In an attempt to salvage the hand, the thumb was amputated at the interphalangeal joint, the index and middle fingers were amputated at the proximal phalanx, and the ring finger was amputated at the distal phalangeal tip with a proximal phalangeal fracture. In an emergency operation, wound debridement and Kirschner wire (K-wire) fixation of the index and ring fingers were performed. All the fingers were open amputated because the stump was lost. The ring finger showed arterial insufficiency, so we anastomosed both digital arteries. One week after the trauma, an angiography was performed to assess the vasculature of the injured hand and revealed an intact radial artery and its dorsal branch (Fig. 1). We subsequently performed a reconstruction using a TDAP free flap to resurface the thumb index and middle fingers. Preoperatively, the perforating artery from the thoracodorsal artery was identified with an audio Doppler machine. The perforating sites were detected, and the most reliable perforating artery was marked. The flap was designed on the basis of the most reliable perforating artery of approximately 18.0×11.0 cm in size. With the identified intermuscular perforating artery from the descending branch of the thoracodorsal artery, a 10-cm-long pedicle was harvested to cover the defect. The flap was harvested with an approximately 1.5-cm thickness by flap elevation excluding the deep adipose layer (Fig. 2). The dorsal branch of the radial artery was identified and used as the recipient artery. Vessel anastomoses were performed end-to-side between the thoracodorsal artery and the recipient artery and end-to-end between one vena comitantes and the cephalic vein. The donor site was closed directly and the flap survived without necrosis or other serious complications. We divided the thumb and the other two fingers 4 weeks later. Finally, we performed debulking and scar excision of the palmar and dorsal sides 3 months later (Fig. 3). The patient was then able to key pinch and grasp objects.
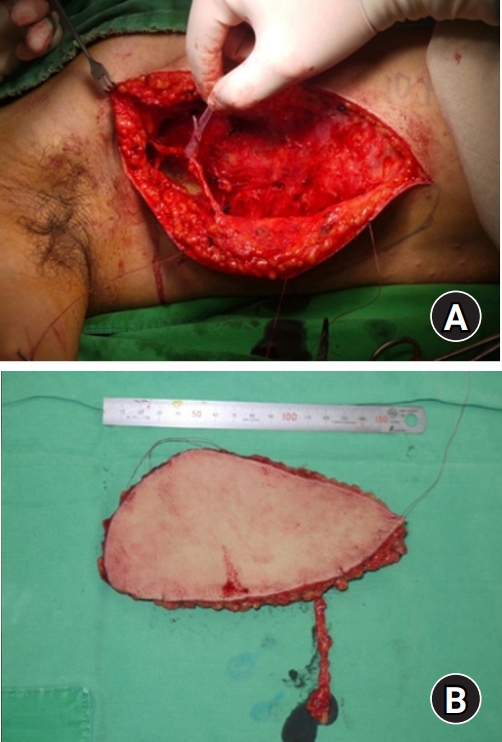
(A) The thoracodorsal artery perforator free flap was designed on the basis of the most reliable perforator of the thoracodorsal artery. (B) An 18.0×11.0-cm flap with a 10-cm-long pedicle is shown.
2. Case 2
A 22-year-old man had a crushing injury involving the thumb, index, and middle fingers of his dominant, right hand due to a power press machine accident. The carpometacarpal joint of the thumb was open-dislocated with the ruptured thenar muscle. The index and middle fingers were fractured and dislocated at the metacarpophalangeal joint, and the distal portion was severely injured. We performed an open reduction and internal fixation with a K-wire of the dislocated carpometacarpal joint of the thumb. The index and middle fingers were amputated because replantation was impossible because of the severely injured status. Then, the thumb showed arterial insufficiency, so we performed microsurgery of the end-to-end anastomosis of princeps pollicis artery to the second common digital artery. The princeps pollicis artery showed an anatomical variation, so it was difficult to identify. Usually, the dorsal branch of the radial artery makes its way into the deep palmar arch by passing through the gap between the first and second metacarpals. The deep palmar arch gives rise to the princeps pollicis artery, which is the main supply artery of the thumb. Therefore, microsurgery for the princeps pollicis artery could be performed on the volar side between the first and second metacarpals. However, in this case, princeps pollicis artery arose directly from the dorsal branch of the radial artery. Then, the dorsal branch of the radial artery passed through under the thumb flexor and A1 pulley. We cut the princeps pollicis artery at the metacarpal area and performed an end-to-end anastomosis to the second common digital artery (Fig. 4). In addition, the ulnar digital artery of the thumb from the index digital artery was not identified. Therefore, anastomosis of princeps pollicis artery is crucial for the survival of the thumb. Partial necrosis of the index and middle metacarpal area developed, so we performed a debridement 4 weeks later. We subsequently used a TDAP free flap for coverage of the thumb, index, and middle fingers. A 15.0×7.0-cm flap was harvested using the same technique in the above-mentioned case. The flap was harvested under a 1-cm thickness by flap elevation, excluding the deep adipose layer. Vessel anastomoses were performed end-to-side between the thoracodorsal artery and the recipient artery and end-to-end between one vena comitantes and the cephalic vein. Postoperative recovery was successful and the flap survived completely. Finally, we performed debulking and a Z-plasty procedure 3 months later (Fig. 5). The patient was able to key pinch and grasp objects with a thin flap.
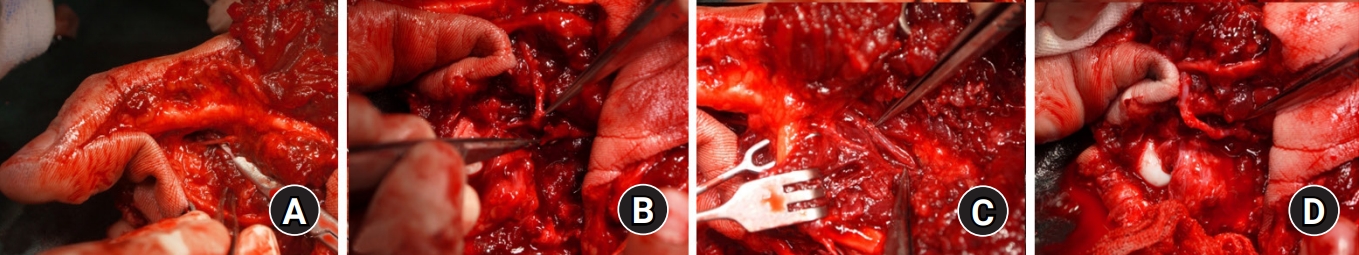
(A) The princeps pollicis artery. (B) The princeps pollicis artery runs through the thumb flexor tendon. (C, D) End-to-end anastomosis between the princeps pollicis artery and the second common digital artery.

(A) Initial injury status. (B) Emergency postoperative status. (C) Partial necrosis developed. (D) Identification of the dorsal branch of the radial artery. (E, F) After the thoracodorsal artery perforator free flap coverage. (G, H) Final debulked status.
Written informed consent was obtained for publication of this case report and accompanying images.
DISCUSSION
Mangled hands are high-energy injuries that are rare and challenging to manage. These injuries usually occur in the workplace and in the healthy young population. Sufficient function of the hands must be restored so that the patient can return to work and perform daily activities. If a staged reconstruction is planned, the decision on the parts to be discarded or salvaged is crucial during the initial surgery. The debridement of contaminated and non-viable tissue, stabilization of the fractures, and replantation of the remaining vessels should be achieved. Then, definitive reconstruction could be performed if the wound is demarcated and no further debridement is necessary. Appropriate soft tissue reconstruction for defects is an important aspect. It not only provides cover for soft tissue defects but also restores function and affects early recovery [4]. Many possible flaps can be used for reconstruction. In our institution, the most frequently used free flaps for hand reconstruction are the radial artery superficial palmar branch perforator (RASP) [5], ALT [1], and TDAP flaps [2,3].
The perforator free flaps have recently been used mainly for the reconstruction of soft tissue defects of the hand [6]. The ALT flap has become popular because it is known to be relatively easy to elevate, have low morbidity at the donor site, and allow broad applicability [1,7]. In the past, the authors usually used RASP and ALT flaps depending on the size of the defects to cover. ALT flaps were mainly used for large defects for which RASP flaps could not be used. However, the authors thought that the ALT flap has the disadvantage of being too bulky for hand reconstruction [6]. The ALT flap with a thinning procedure or superficial fascial elevation can be performed with removal of a considerable amount of deep fatty tissue however, it may cause partial flap necrosis and is technically demanded [1]. The TDAP flap could be a reliable option to substitute the ALT flap [2,3,8]. The main reason for selecting the TDAP free flap is its thinness and the less exposure of the donor site in the back for resurfacing. The back has superficial and deep adipose layers comparing with the thigh [8]. The TDAP flap can be harvested at a thickness of approximately 5 mm to 1 cm by flap elevation, excluding the deep adipose layer [8]. A thin flap facilitates rapid sensory recovery and the earlier recovery of the abilities to pinch and grasp [3]. It was reported that ALT flaps can be thinned to a thickness of approximately 3 to 4 mm [1]. Depending on the surgeon’s proficiency and the patient’s own fat layer, the superiority of thinness between ALT and TDAP is thought to be controversial.
Compared with other flaps, the TDAP flap has additional advantages in that the donor site on the back is less exposed and wider flap harvesting is possible. All donor muscles and nerves can be preserved, the pedicle length can be easily controlled and large flap dimensions of up to 20×10 cm can be elevated with simple primary closure [8]. Several perforator free flaps can be harvested from the back, such as the circumflex scapular artery perforator flap [9]. However, this flap should be harvested in the prone position. The TDAP flap could be applied without intraoperative changes in position. In addition, the area of the drape is narrow, as it is performed near the back of the ipsilateral side of the hand reconstruction. The narrow drape could be related to the low infection rate and convenience of operation for surgeons.
The TDAP flap was thought to be quite difficult and time-consuming to elevate. After several trials, it is no longer as difficult as previously experienced, even though the TDAP flap takes less time to harvest than the ALT flap because of its short transmuscular dissection through the thin latissimus dorsi muscle [2].
The second case showed an anatomical variation of the princeps pollicis artery (Fig. 6). The princeps pollicis artery is the main feeding vessel of the thumb, which usually branches from the deep palmar arch. An anatomical variation in the location where the princeps pollicis artery would branch was reported. In some rare cases, the princeps pollicis artery branches from the superficial palmar arch or the dorsal branch of the radial artery. The princeps pollicis artery supplies the dominant blood flow to the thumb. It is important in microsurgery because of the lack of collateral blood flow [10]. Microsurgeons should consider the anatomical variation of the princeps pollicis artery when performing thumb replantation.
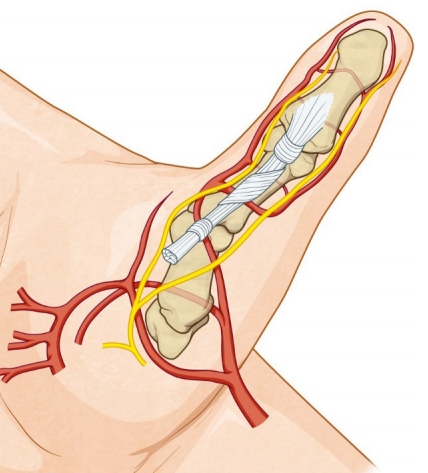
The princeps pollicis artery directly branches from the dorsal branch of radial artery, then passes through under the flexor tendon.
As described earlier, successful reconstruction of mangled hands was possible using TDAP free flaps. The TDAP flap is suitable for hand reconstruction because of its short transmuscular course and large flap with easy primary closure. The results showed an aesthetically acceptable scar, early functional recovery, and minimal donor site morbidity. Owing to these advantages, a TDAP free flap can be a reliable option for soft tissue reconstruction of the hand.
Notes
The authors have nothing to disclose.


