Sesamoid arthritis with locked metacarpophalangeal joint misdiagnosed as trigger finger: a case report
Article information
Abstract
Locked metacarpophalangeal joint (MCPJ) is mainly caused by joint pathologies, although tendinopathy is also a possible cause. Furthermore, it can be misdiagnosed as tendinopathy with triggering symptoms. Herein, we present a 60-year-old housewife with thumb flexion inability lasting for 4 months. Three weeks previously, she visited another clinic and was misdiagnosed with trigger thumb. Her symptoms did not resolve after trigger thumb surgery. At our clinic, physical examination and imaging studies were conducted. Sesamoid arthritic change with entrapment in the MCPJ was found, and the entrapped sesamoid bone inhibited flexion of the MCPJ of the thumb. Based on the examinations, radial sesamoidectomy was planned. After surgery, the patient recovered a passive full range of motion immediately. Despite a rehabilitation program, at 6 months postoperatively, severe stiffness and contracture at the MCPJ were noted. Therefore, a second operation with tenolysis and volar plate release was conducted under wide-awake anesthesia. Intraoperatively, severe adhesion was observed in flexor tendon, volar plate release was performed, and small defects were found in the volar plate when thumb was fully extended. To prevent secondary healing of the volar plate defect, a dorsoradial adipofascial flap was used. At 6 months after the second surgery, the patient’s range of motion in the MCPJ had improved, and she resumed activities of daily living without other complications. Hand surgeons frequently misdiagnose conditions as trigger finger if there is triggering or locked-joint symptoms. An accurate preoperative diagnosis with a detailed physical examination and imaging studies are essential for better operative results.
Introduction
The sesamoid bone is a small-rounded bone that looks like a sesame seed. It was first identified by Galen [1]. The incidence of the sesamoid of the metacarpophalangeal joint (MCPJ) of the thumb ranges from 98% to 100% [1]. The function of the sesamoid bone is not clearly known yet. Previous studies have several hypotheses, it is a part of the flexor gliding mechanism that reduces friction power, protects the joint from trauma, and stabilizes the flexor tendon of the thumb [1].
There are various sesamoid pathologies. It contains trauma, degenerative changes, tumors, etc. Sesamoid disorder is most commonly attributed to trauma [1]. However, sesamoid fracture is rarely reported and is usually associated with strong hyperextension forces or direct trauma [2,3]. Sesamoid fracture or severe comminuted fracture of the sesamoid bone can cause sesamoid arthritic change. Further, arthritic change in the sesamoid joint with the metacarpal bone can lead to loss of range of motion and pain. Moreover, it can be misdiagnosed as other diseases such as trigger thumb [4]. In this article, we present a case of sesamoid arthritis with locking of the MCPJ of the thumb caused by falling and direct forces on the radial sesamoid bone.
Case report
The Institutional Review Board of Korea National Institute for Bioethics Policy (KoNIBP) approved this case report (No. P01-202307-01-019). The patient provided informed consent for the publication of the clinical photographs included in this article.
A 60-year-old housewife with thumb flexion inability for 4 months visited our clinic. The patient’s symptom started after the patient slipped down and her hands were forcefully placed on the ground. There are not any previous traumas on her hands. She visited other hand clinics, and the condition was misdiagnosed as trigger thumb based on subjective symptom alone (inability to perform active flexion of the thumb) without any additional studies. However, her symptoms did not resolve after trigger thumb surgery despite the encouragement of postoperative rehabilitation.
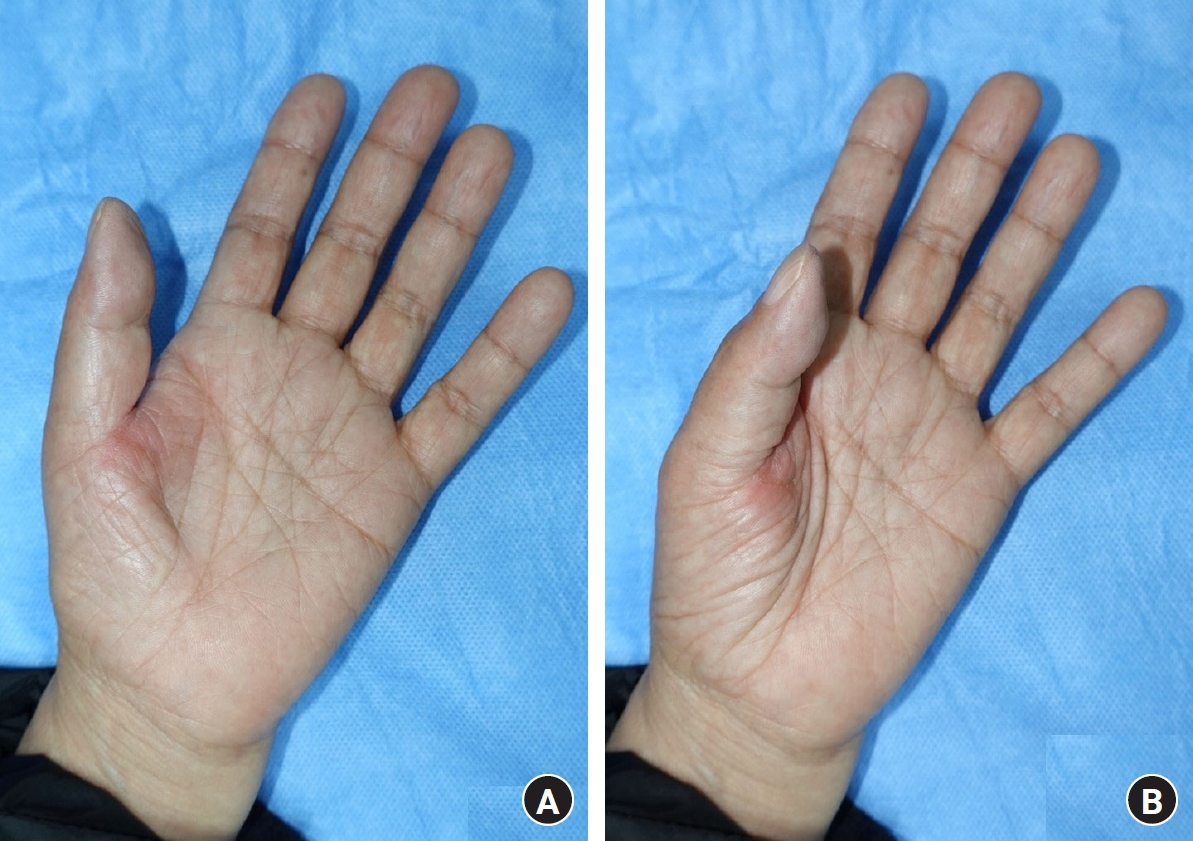
Based on physical examination, the patient cannot flex her thumb actively, and the MCPJ of the thumb could not be flexed passively. Further, the interphalangeal joint of the thumb was fixed at 20° in flexion (Fig. 1). The patient complained repetitively about her inability to flex the MCPJ and the rigidity of the previous operative site.
Although the A1 pulley released was conducted in another clinic, the MCPJ could not be flexed, which means the mechanical blocking of flexion of the MCPJ of the thumb. Plain radiography revealed deformity of the sesamoid bone of the MCPJ of the thumb. A computed tomography (CT) scan and magnetic resonance image (MRI) showed a sharp deformity via the MCPJ joint, which looks like a bird beak. In addition, there are slightly prominent metacarpal heads without any other deformity in MRI (Fig. 2). The “bird-beak” deformity inhibited flexion of the thumb (locked MCPJ). Ultrasonography showed the rough surface of the radial sesamoid bone with adhesion of flexor tendon. We performed sesamoidectomy and exploration of the flexor tendon.

Preoperative imaging studies. (A) Plain radiography showed deformity of the radial sesamoid bone and a bone fragment around the metacarpophalangeal joint (MCPJ). (B) Computed tomography scan and magnetic resonance imaging revealed a bird beak-shaped radial sesamoid bone and entrapment in the MCPJ, which caused mechanical MCPJ blocking.
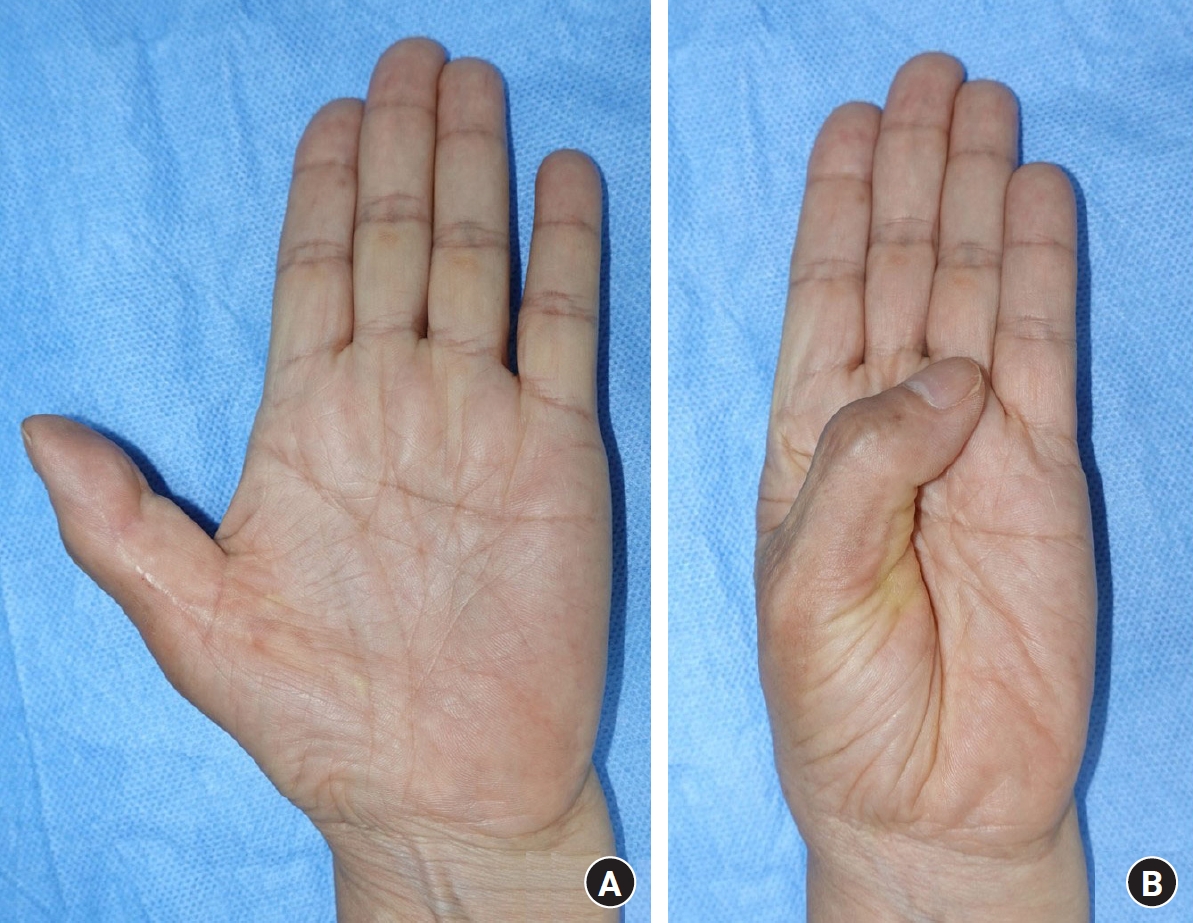
Intraoperatively, under brachial plexus block, severe adhesion and scar formation were observed around the flexor tendon. Further, the patient presented with digital nerve swelling and scar formation which can result in traction neuritis. Digital nerve neurolysis, flexor pollicis longus tenolysis, and radial sesamoidectomy were performed, and the patient immediately recovered her passive full range of motion of the MCPJ. The resected bone presented with an extremely sharp and decorticated, denuded surface, and it might present as a fracture and malunion of the sesamoid bone (Fig. 3). After 7 days postoperatively, early rehabilitation program was started, the compliance in rehabilitation was fine.
(A) Inability to flex the metacarpophalangeal joint (MCPJ) of the thumb. (B) The radial sesamoid bone with arthritic changes was resected. (C) After radial sesamoidectomy and tenolysis, the patient recovered a passive range of motion in the MCPJ of the thumb. (D) Severe decortication and arthritic changes in the sesamoid surface were observed on the articular side (above) and the volar side (below).
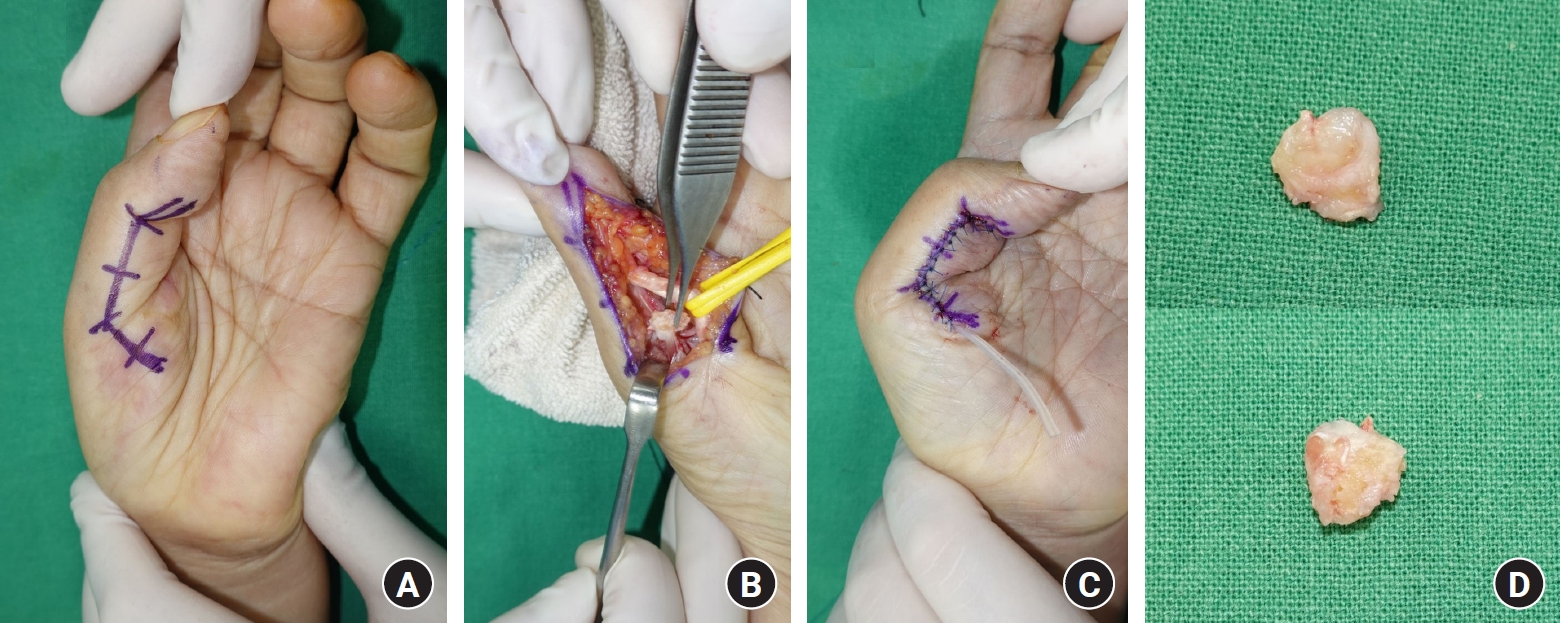
At 6 months postoperatively, stiffness, and contracture were observed in the MCPJ. The range of motion of the MCPJ was almost at 5°. Severe flexor adhesion and volar plate contractures were noted on ultrasonography. Therefore, tenolysis and volar plate release were performed under wide-awake anesthesia. After the volar plate release, there were small defects on the volar plate. The dorsoradial adipofascial flap was used to prevent the secondary healing of volar plate defects. Full active flexion of the MCPJ and mild extension lag of the interphalangeal joint of thumb were achieved (Fig. 4).
(A) Limited range of motion of the thumb during extension (left) and flexion (right) before the third surgery. (B) Tenolysis of the flexor tendon with severe adhesion and tendon thickening. (C) Adipofascial flap elevation for the volar plate defect. (D) Postoperative range of motion (extension [left] and flexion [flexion]) of the thumb under wide-awake anesthesia.
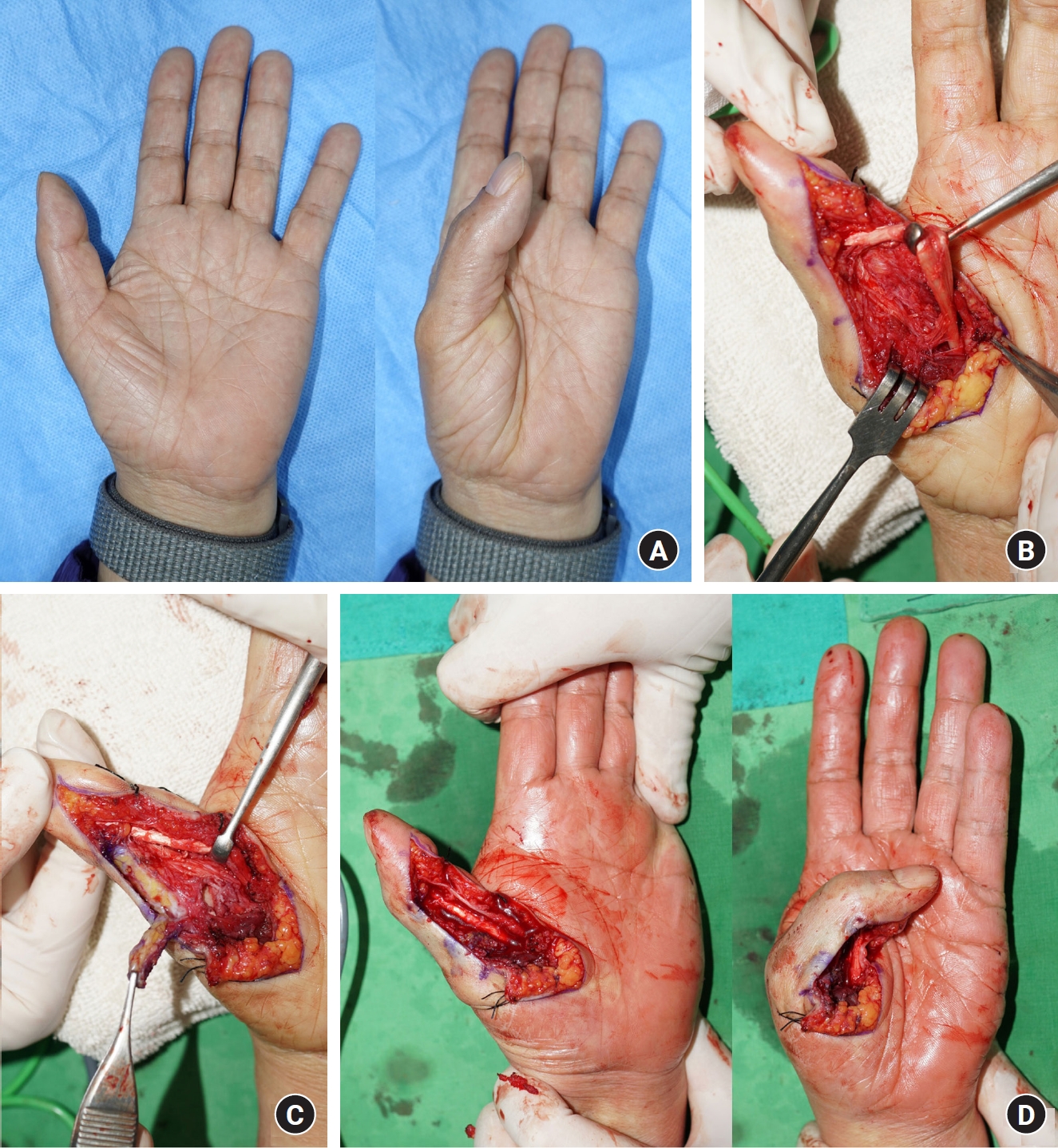
The postoperative course was fine. The patient received a continuous and passionate rehabilitation program. At 6 months after the second surgery, the range of motion of the MCPJ improved (0°–35° for actively, 0°–55° for passively), and the patient resumed activities of daily living without other complications (Fig. 5).
Discussion
The locked MCPJ of the thumb has been rarely reported previously. Tendon and joint problems are the two possible main pathologies of locked MCPJ. Locked joints are more likely to be caused by joint rather than tendon pathologies. Severe trigger thumb is the main tendinopathy causing locked joint, and arthritic change of the MCPJ and sesamoid entrapment are primary joint problems associated with the condition. Sesamoid pathology has been found to be related to the locking of the MCPJ of the thumb, and it requires strong hyperextension forces with traction and rotation forces of the MCPJ of the thumb [5,6]. Trigger thumb, known as stenosing flexor tenosynovitis of the A1 pulley, can cause locking of the thumb, swelling, and thickened flexor tendon entrapment through the A1 pulley [7].
Trigger thumb with locked joint can be treated with A1 pulley release with tenosynovectomy, and the locked MCPJ can be treated with open reduction and ligament repair or sesamoidectomy. Some studies have shown that the quadrilateral-shaped metacarpal head was vulnerable to sesamoid entrapment, sesamoidectomy was recommended for quadrilateral-shaped metacarpal head (metacarpal groove-like depression). However, the indication for sesamoidectomy was not clearly established yet [6,8,9].
In our case report, sesamoid entrapment was attributed to the “bird-beak” shape deformity of the radial sesamoid with arthritic change. Considering the patient’s trauma history, the condition could have been caused by sesamoid fracture or sesamoid dislocation in the MCPJ. However, locked MCPJ started immediately after the patient slipped. Further, some bony fragments around the radial sesamoid and severely distorted shape of the sesamoid bone itself were observed. Hence, the condition was believed to be caused by a sesamoid fracture. The sesamoid fracture is rare; only a few case reports were reported [2,3]. In addition, there are several case reports about sesamoid arthritis, but there are not any reported cases that showed sesamoid arthritis with locked MCPJ [4]. At the previous another clinic visit, the patient underwent surgery with A1 pulley release. Nonetheless, the locked MCPJ did not resolve. Hand surgeons often overlook MCPJ pathologies including sesamoid pathologies, particularly those related to triggering symptoms [4]. Therefore, simply the locked MCPJ does not misdiagnose for tendon entrapment.
Intraoperatively, a severe decorticated, and sharply contoured sesamoid was observed. Locked MCPJ did not resolve with reduction alone, and sesamoidectomy was needed for arthritic change in the sesamoid bone with deformity. There are two noteworthy points in our case, the first point was the postoperative severe adhesion and contracture on the MCPJ of thumb. The duration from the first surgery with A1 pulley release to sesamoidectomy was only 3 weeks. Thus, severe scar tissue formation and fibrosis were observed. Evidence-based surgical treatment was important. Surgical treatment based on misdiagnosis and prolonged problems shorten intervals until reoperation, which makes severe adhesions and contractures. The second point was the necessity of volar plate release. After sesamoidectomy, the patient presented with severe volar plate contracture and flexor tendon (flexor pollicis longus) adhesions, in the second surgery, tenolysis and volar plate release were performed, and volar plate defect was identified. The secondary healing process of the volar plate is not ideal because it can cause recurrent volar plate contracture. Hence, the adipofascial flap was used. After performing tenolysis and arthrolysis, the range of motion of the MCPJ of the thumb improved. There are several case reports that improved locked MCPJ after sesamoid bone resection, however, in this case, locked MCPJ was resolved by performing volar plate release additionally after sesamoid resection. This point does not suggest the necessity of routine volar plate release. When there is severe adhesion, longstanding contracture and volar plate injury due to inappropriate trigger thumb surgery, if the reoperation was necessary, volar plate release can be considered as a surgical option after sesamoidectomy with insufficient symptoms improvement.
Herein, we present a unique case of locking of the MCPJ of the thumb with sesamoid arthritis misdiagnosed as a trigger finger. Locking or triggering symptoms of the thumb are commonly misdiagnosed as stenosing tendinopathy, and hand surgeons frequently overlook joint pathologies. There are various preoperative image modalities that can be helped in obtaining differential diagnosis (MRI, CT, ultrasonography, etc.). Although CT was first considered for diagnosis of sesamoid arthritis, however, we suggest that ultrasound should be first considered for an accurate diagnosis. Ultrasonography is a noninvasive, inexpensive, and dynamic modality for preoperative diagnosis and is essential for obtaining differential diagnosis in patients with tendon or MCPJ issues. A few studies have assessed the need for ultrasonography for sesamoid entrapment [10]. Based on the ultrasound, additional tests including MRI or CT can be performed if necessary. An accurate preoperative diagnosis with detailed examination enables to avoidance of postoperative complications.
Notes
The authors have nothing to disclose.
Funding
None.