악성말초신경피복종 절제 후 발생한 광범위 등 결손의 등늑간동맥 천공지 프로펠러 피판술을 이용한 재건: 증례보고
Propeller Dorsal Intercostal Artery Perforator Flap for an Extensive Defect on the Back Following Malignant Peripheral Nerve Sheath Tumor Resection: A Case Report
Article information
Trans Abstract
Posterior trunk defects have been a challenging anatomical area to cover in reconstructive surgery. The use of local myocutaneous flaps has been described extensively in the literature to cover these defects, but these techniques are associated with significant donor-site morbidity, including functional loss of muscle units. Freestyle perforator flaps enable local tissue recruitment with skin of a similar color and texture in diverse anatomic areas, but there is a shortage of case series on posterior trunk defects using propeller dorsal intercostal artery perforator (DICAP) flaps, particularly when the defects are extensive. In this report, the authors present a successful case of a DICAP propeller flap for an extensive defect on the upper back following a malignant peripheral nerve sheath tumor resection.
INTRODUCTION
Posterior trunk defects result from diverse etiologies, such as pressure sores, tumor resection, infection, or trauma, and represent a challenging procedure. Myocutaneous flaps, such as the latissimus dorsi flap or trapezius flap, have been widely used to cover these defects [1-3]. Although these flaps are preferred by some authors because of simple and reliable techniques [4], they are associated with greater donor-site morbidity than perforator flaps.
The introduction of perforator flaps [5] has revolutionized reconstructive surgery over the past two decades. The application of perforator flap technique enables long and reliable vascular pedicles, thinner flaps with minimal donor-site morbidity and without including muscle tissue [6]. Intercostal artery perforator flaps have been used widely to cover the diverse trunk defects, based on an understanding of the anatomy of intercostal vessels [7-12]. Among them, dorsal intercostal artery perforator (DICAP) flaps have recently been described in posterior trunk reconstruction [13-17].
This paper describes a case of a large DICAP propeller flap for the reconstruction of extensive posterior trunk oncological defects.
CASE REPORT
The patient was a 70-year-old woman with neurofibromatosis I (von Recklinghausen’s disease) with the chief complaints of a giant mass on her left upper back that had been increasing in size gradually for 10 years (Fig. 1). Preoperative computed tomography showed a lesion, measuring 20×15×10 cm3, overlying the trapezius muscle and the infraspinous region of the scapula. Under general anesthesia, a wide local excision of the lesion was performed with a 2-cm margin. Frozen sections of the excision margins were free of tumor. The tumor was excised at a submuscular plane, including the trapezius, rhomboid major and minor, directly below the tumor. The soft tissue defect was approximately 25×20 cm2 in size and a 30×18-cm2 DICAP propeller flap was designed to close the defect based on the 6th posterior intercostal artery (Fig. 2). An exploratory incision was made, and a large perforator was identified (Fig. 3). The perforator flap was elevated at the subfascial level and transposed 90° into the defect. The donor site was closed directly and the remaining wound was covered with a split-thickness skin graft (Fig. 4). The flap healed uneventfully. Histopathology demonstrated a completely excised malignant peripheral nerve sheath tumor (MPNST). At 6 months postoperatively, the patient did not have any limitation in the range of motion or pain (Fig. 5). Written informed consent was obtained for publication of this case report and accompanying images.

A 70-year-old female with a malignant peripheral nerve sheath tumor measuring 20×15×10 cm3 was present on the left upper back.
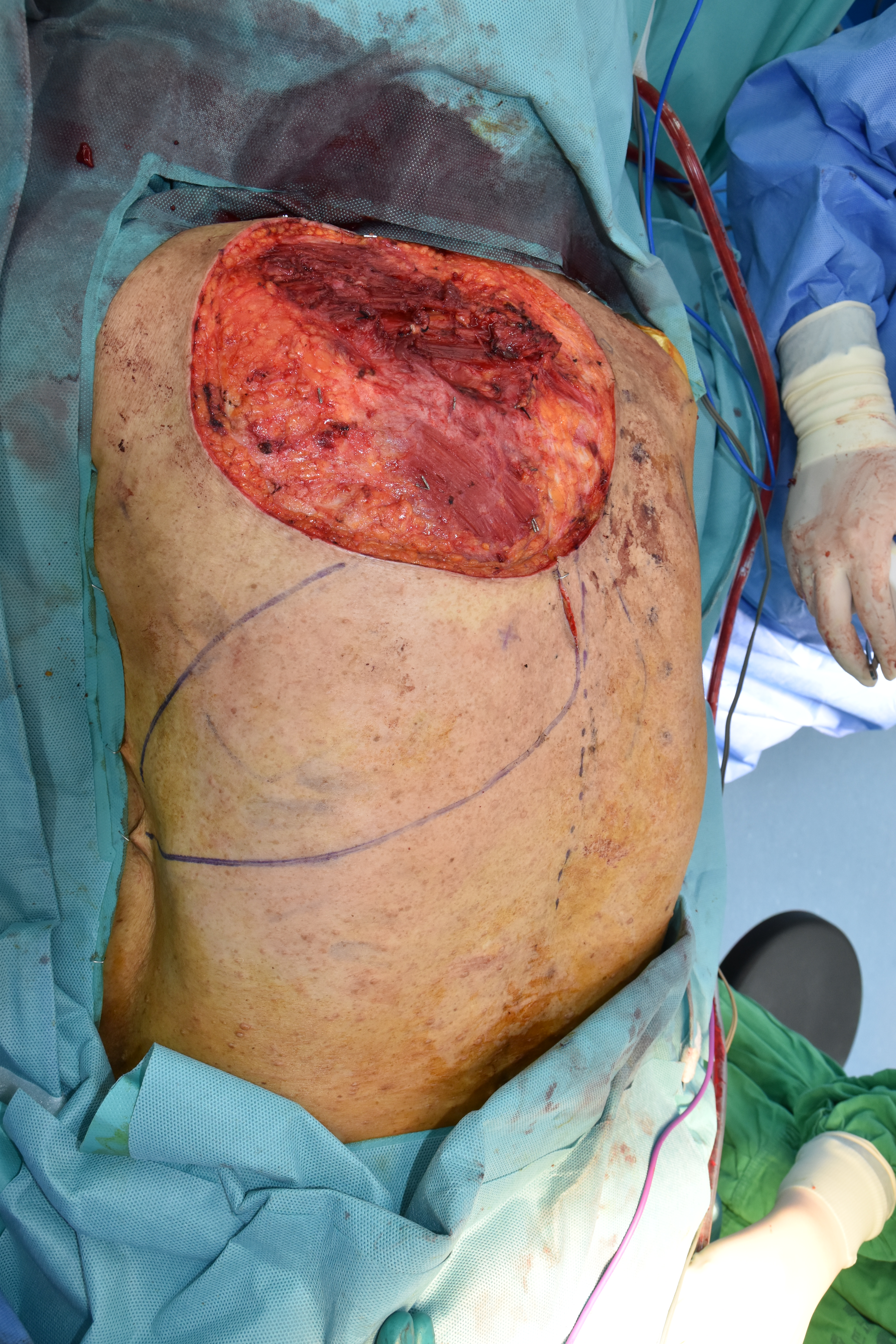
Wound defect after wide local excision of malignant peripheral nerve sheath tumor that measured 25×20 cm2. A 30×18-cm2 propeller dorsal intercostal artery perforator flap was designed to close the defect based on the 6th posterior intercostal artery.
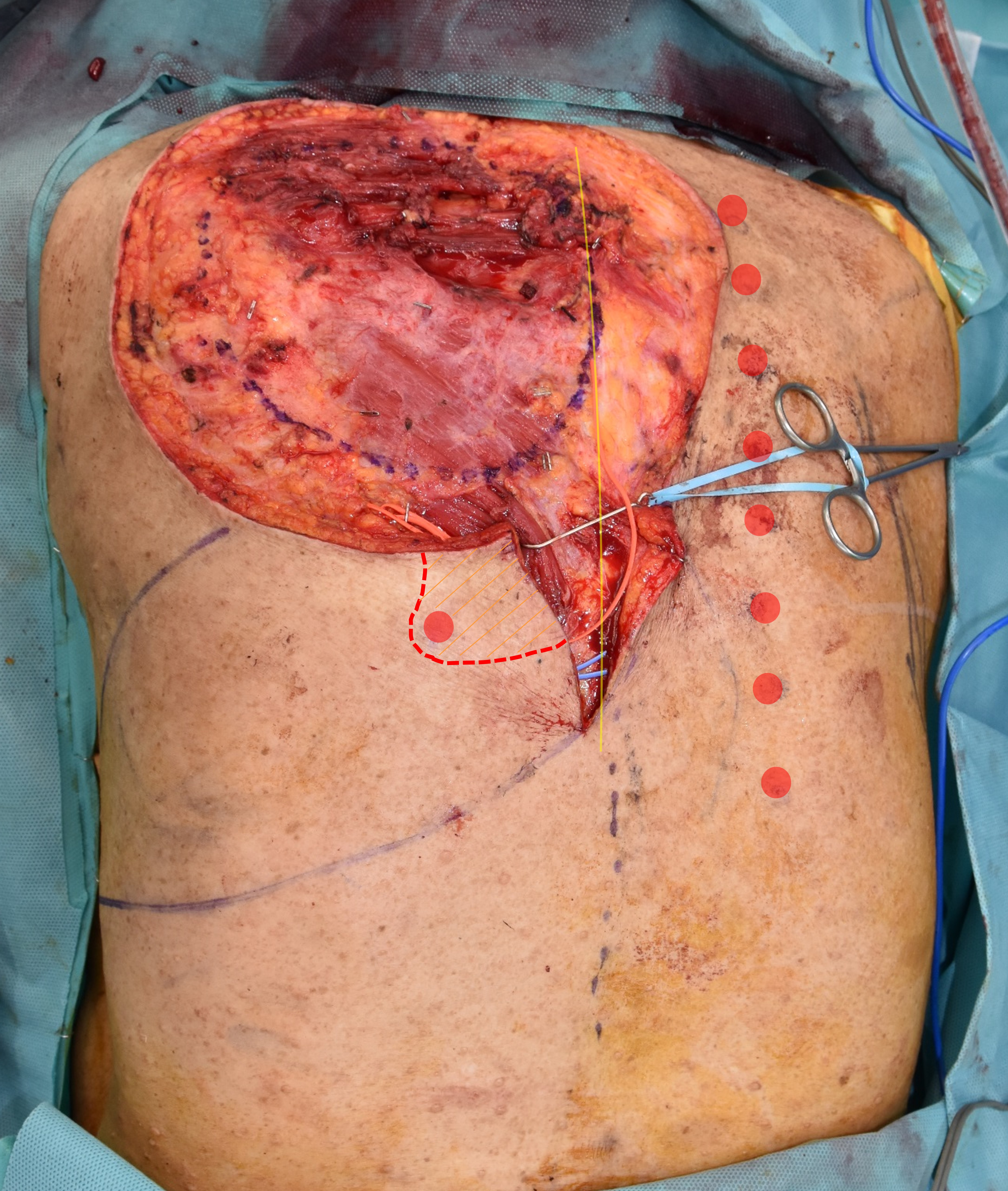
The 6th posterior intercostal artery was identified using an exploratory incision adjacent to the defect. Red circles, preoperative localization of the posterior intercostal artery perforators using a hand-held Doppler; red dotted line, the course of the vessel loop around the 6th posterior intercostal artery under the flap; yellow line, the midline; orange shaded area, the elevated flap area.
DISCUSSION
Posterior trunk reconstruction may be a challenging procedure. Many different operative options have been used to cover the posterior trunk defect; each has distinct advantages and disadvantages. Myocutaneous flaps, such as the latissimus dorsi flap and the trapezius muscle flap, have long been the main treatment for posterior trunk reconstruction [1,2,18,19]. These flaps provide well-vascularized tissue and simple and reliable techniques, but they imply major donor-site morbidity (sacrifice of a major muscle), increased blood loss, and longer operative time. As a consequence, posterior trunk reconstruction has been addressed with perforator flaps, such as the thoracodorsal artery perforator flap or the intercostal artery perforator flaps [9,19].
There are multiple perforating vessels in the dorsal area, and the anatomy of intercostal vessels has been studied extensively [7]. The DICAPs arise from the posterior intercostal artery at the vertebral segment. Consistent with the angiosome theory and recently published studies [20], the DICAP flap can be extended safely to capture adjacent perforasomes because of the extensive true anastomotic connections with the multiple surrounding perforators [10]. To date, the biggest DICAP flap elevated on a single perforator reported thus far was a 40×15 cm2 propeller flap by Prasad and Morris [17].
The size of the flap in the present case was slightly smaller (30×18 cm2), but it extended from the posterior midline to approximately the midaxillary line based on a single perforator. The flap was elevated safely and healed uneventfully without tip necrosis or congestion. There were some technical points and originalities with satisfactory results. First, MPNST is biologically an aggressive tumor, and its excision is difficult because of the intractable hemorrhage. Maintaining a bloodless field is paramount to ensuring clear visualization of the perforating vessels and safe excision. To accomplish that, a wide local excision of the lesion was performed with a 2-cm margin three-dimensionally, not only for the tumor clearance but also for the inclusion of normal tissue for less bleeding. In addition, an MPNST excision is performed with the generous use of bipolar electrocautery. Second, an exploratory incision (4 cm) was made first, and a perforator adjacent to the defect was explored. After identifying the large perforator, the skin islands were redesigned according to the perforator location and the size of the defect. The isolated perforator is mobilized and dissected free with the overlying to prevent flap congestion and to gain sufficient pedicle length without tension. According to the anatomical study and clinical applications of DICAP flap [16], it could safely be extended as far as the midaxillary line or the anterior border of the latissimus dorsi with stable blood circulation and complete survival.
As described above, successful reconstruction of the back was possible using a DICAP propeller flap. Although there is a limitation that requires long-term follow-up, a DICAP propeller flap offered a satisfactory result in the present patient. Overall, this technique offers early recovery with minimal donor-site morbidity.
Notes
The authors have nothing to disclose.
Acknowledgements
This work (research) was supported by Chungnam National University Hospital Research Fund, 2018 (2018-CF-026). This research was supported by Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Science, ICT, & Future Planning (NRF-2018R1A2B6007425).


