|
 |
- Search
| Arch Hand Microsurg > Volume 25(4); 2020 > Article |
|
Abstract
Scalp amputation is a very rare occurrence worldwide. In particular, replantation failure may occur from venous congestion, which represents a major complication of replantation. Accordingly, this study reports on a scalp amputation case with successful replantation treatment using medicinal and chemical leech therapy. On November 11, 2017, a 47-year-old female patient experienced a complete amputation injury starting from the top of the nose involving the total scalp by rolling machine that packs laundry. Severe venous congestion was controlled by medicinal leech therapy performed six times a day and chemical leech therapy (subcutaneous low-molecular-weight heparin injection) three times a day for 10 days. Approximately 85% of the scalp was replanted, and hair growth was confirmed. The basic concept of replantation surgery, “replace tissue with like tissue,” makes replacement impossible with tissues other than the hair-bearing scalp. Accordingly, the authors present a case of successful replantation with both medicinal and chemical leech therapy.
Total scalp amputation is relatively rare worldwide. Avulsion of the scalp most commonly results from the entrapment of long hair in high-speed rotary parts of industrial machinery. Avulsion injuries differ from cutting injury in terms of having an extensive region of trauma and inducing significant vessel injury, making the microvascular replantation more cumbersome. In scalp avulsion injuries, traction forces lead to serious vessel damage including the intimal wall, which in turn is highly thrombogenic.
The first scalp replantation for total scalp avulsion was performed by Miller et al. [1] in 1976. Acute management of an avulsed scalp, before the advent of microsurgical techniques, typically involved simply replacing the avulsed portion as a free graft and suturing it back in place. Microsurgical replantation is the best reconstructive technique following total scalp amputation. Although 60 to 70 scalp amputation cases had been reported, most of the studies had small samples [2-4]. Most of the authors advised that no hair-bearing autologous tissues that substitute scalp exists and the best surgical results are achieved with a greater number of sutured arteries and veins [5]. Venous congestion of regional and free tissue transfers is a common cause of flap failure even if a successful microsurgical anastomosis is done. This complication can be related to several contributing factors, such as intrinsic venous anatomy, absence of venous repair, venous spasm, venous thrombosis, local edema, pedicle torsion, among others [4,6]. Insufficient venous anastomosis is known as the most common reason for replantation failure [3,7-8]. Thus, the availability of a reliable vein for drainage is the key to successful microvascular replantation [5].
Many authors considered medicinal leech therapy (MLT) as one of the first choices for the treatment of flaps [9]. Thus, this study proposed a successful protocol for the management of severe venous congestion after microanastomosis with MLT followed by chemical leech therapy injecting 2-mg subcutaneous low-molecular-weight heparin (LMWH) three times a day for 10 days.
A 47-year-old woman presented to the hospital with a complete amputated scalp after her hair was caught in a laundry-packing machine. Compact compression dressing with gauze and elastic band was applied, owing to severe bleeding by completely ruptured both superficial temporal artery (STA) and superficial temporal vein (STV) (Fig. 1). The laceration extended across the total scalp, forehead, both supratarsal fold, and levels I and II neck.
Upon arriving at the hospital, the patient received an initial evaluation and was stabilized in the emergency room. The patient was immediately transported to the operating room after examination and exclusion of any other associated life-threatening injuries. The amputated scalp was rinsed with saline, and the total ischemic time was approximately 4 hours. The surgical procedures were performed under general anesthesia and distal vessels were identified under an operative microscope. The STA and veins were identified on the scalp first. Bilateral temporal arteries and veins were used as recipient pedicles. The temporal artery was dissected proximally in the patient and distally in the flap to mobilize as much length as possible for the reanastomosis. The left STA and STV were narrow and short, and additional anastomosis resulted in less blood flow without the use of vein graft. Thus, the vein graft was performed on the left temporal vein using the right posterior tibial vein with exploration.
MLT (three to four leeches per time) was performed four to six times a day to relieve venous congestion to maintain blood flow, and chemical leech therapy of 2-mg subcutaneous LMWH (40 mg of enoxaparin sodium; Clexane, Sanofi, Paris, France) was injected three times a day for 2 weeks after reanastomosis to manage severe venous congestion (Fig. 2). Continuous heparin-mixed wet saline gauze dressing was applied to prevent wound crust. The patient was massively transfused with packed red blood cells 5 days after reanastomosis with vein graft (mean volume, 1.12 L/day) and 4 more days thereafter (mean volume, 1.1 L/day). The mean drainage volume (three drains on the scalp area and one drain on the neck area) after initial reanastomosis was 922.5 cm3 (range, 300 to 1,540 cm3) on the scalp area and 122.5 cm3 (range, 75 to 170 cm3) on the neck area until secondary operation. One negative pressure drain on the scalp area remained during the vein graft. The initial drain was 1,600 cm3, which reduced gradually until 12 days postoperative removal (mean volume, 290 cm3; range, 10 to 1,600 cm3). The patient also underwent debridement twice and irrigation including wound revision during the period.
The scalp mostly survived. However, partial skin necrosis developed in the lower left occipital area region. Therefore, the lesion was debrided and reconstructed with a split skin graft 2 weeks after the operation. Exuberant hair was evident 2 months after the first operation, but the patient’s hair growth pattern was different on the sides. The right temporal area had greater hair growth compared with the occipital and the left temporal area of the scalp. At 3 years postoperative, hair had grown sufficiently in the rest of the scalp; approximately 85% of scalp flaps except the lower left occipital area of the scalp (Fig. 3). Several scar revisions were done on the neck and eyebrow for better aesthetic outcomes during 2 years postoperative.
Written informed consent for publication of the clinical images was obtained from the patient.
The scalp is a unique body structure that consists of densely packed hair follicles, a thick subcutaneous layer, and neurovascular bundles. Before the advent of microsurgery, the exposed calvarium was treated by the skin graft method, which often led to baldness. The first scalp replantation was performed by Miller et al. [1] in 1976.
Scalp replantation is a relatively rare occurrence, and the current case was a one-piece amputation starting from the top of the nose, crossing the upper tip of both ears, and extending down to the lower occipital area. Severe venous congestion was observed throughout the flap owing to increased artery-to-vein ratio before vasculogenesis. An MLT of six times per day and chemical leech therapy of 2-mg subcutaneous LMWH injection three times per day were performed for 10 days with wet heparin dressing to keep tissue viability and minimize hair loss in the flap. Each day number of MLT was lessened as the flap condition went less congestive (Fig. 4). Partial blenching on flap started to be observed at postoperative day 10, of which area expanded through the flap as time progressed.
An interposed vein graft from the right tibial vein was done to provide sufficient length because the injured left temporal vein was inadequate for a tension-free anastomosis. In the literature, some studies suggest that one artery and one vein anastomoses are sufficient for scalp perfusion [3]. Similarly, Nguyen [7] demonstrated in a series of seven scalp avulsions that the amputated part can be sufficiently perfused by single artery anastomosis due to the robust collateral flow in the scalp as long as the galea is intact. However, some studies also suggest the necessity of multiple anastomoses [3]. In this case, partial skin necrosis only developed in the lower left occipital area. As demonstrated by three-dimensional computed tomographic angiography 4 months postoperative (Fig. 5), only the right STA and STV showed blood flow, while the left STA and STV could not be enhanced, suggesting that the entire scalp had circulation via the right STA and STV with occlusion on the left side. These findings may reflect the alopecia on the lower left occipital area of the scalp where the skin graft was done to prevent further hair loss. Focal alopecia was aesthetically complemented because the other parts of the hair grew.
No hair-bearing autologous tissue can substitute the scalp. Thus, a successful replantation of the avulsed scalp flap is the first step. The majority of the reported cases of occipital congestion seem to be due to postoperative venous congestion. This is likely a result of two factors (the small caliber of the occipital vessels and the difficulty in finding and using them in the anastomosis and the gravitational dependence of the area). This specific complication can be lessened by MLT followed by chemical leech therapy injecting 2-mg subcutaneous LMWH. Reports in the literature show an onset of action around 2 hours postinjection, reaching its maximum at 4 to 5 hours with a period of action up to 12 to 24 hours, even though the subcutaneous bioavailability of LMWH in the congestive segment may vary. Local subcutaneous heparin injection was first reported by Barnett et al. [9] in 1989 as an effective treatment for venous congestion in digital replantation [10]. Furthermore, Pérez et al. [10] discussed the application of this therapy with an established protocol regarding the dose, frequency of administration, and duration of treatment. Despite the occlusion on the left temporal vessels, approximately 85% of the scalp area has shown viability with thick hair growth with the proposed therapy and additional skin graft.
Volume management may be challenging due to the continuous venous oozing for several hours following LMWH therapy, and blood loss may be underestimated. It is therefore essential to frequently check the patients’ vital signs and hemoglobin levels and transfuse properly. Transfusion requirements will be directly related to the severity of flap venous congestion and the size of the congested area. Drainage insertions in recipient sites to prevent hematoma is considered to be an additional risk related to postoperative anticoagulant use.
In conclusion, local subcutaneous LMWH injection is an available and easily applicable therapy for regional and free congested flaps. In this case, MLT was added before LMWH. Avulsed scalp appeared to be viable in over 85% by this protocol, though with severe postoperative venous congestion and left temporal vessel occlusion.
Fig. 1.
Preoperative findings. (A) Completely amputated defect on the scalp area. (B) Amputated stump.
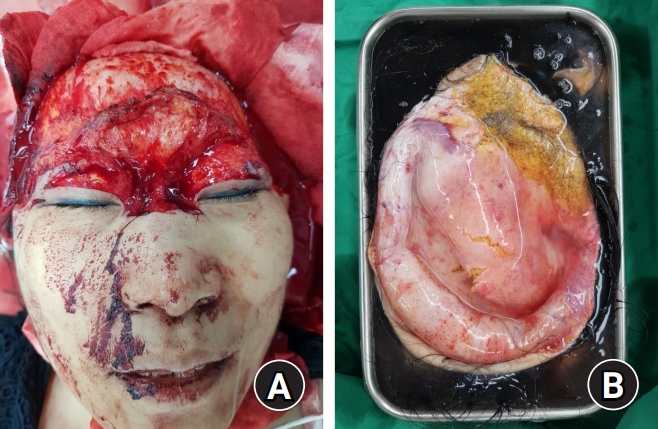
Fig. 2.
Severe venous congestion on the replanted scalp on postoperative day 2. (A) Anterior-posterior view, (B) left lateral view, and (C) crown view.

Fig. 3.
Postoperative findings after microsurgical replantation after 2 weeks (A), 6 weeks (B), and 4 months (C). Follow-up observation was performed while continuing leech therapy. Venous congestion was improved in postoperative day 5, and wound healing was almost completed at 2 weeks postoperative. The views of anterior-posterior (D) and posterior-anterior (E) after 3 years. Hair growth is observed in approximately 85% of scalp flaps.
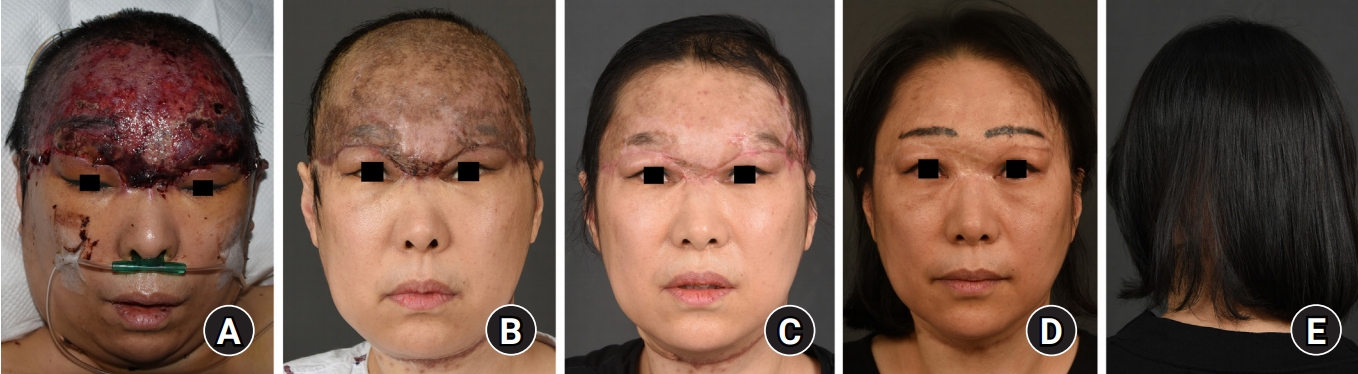
Fig. 4.
Postoperative pack cell transfused, post-transfusion hemoglobin level, flap color, and conducted medicinal and chemical leech therapy protocol. The hemoglobin level maintained above 7 g/dL and congestive flap color resolved in length of time. The flap color is shown at the most congestive point in each period. The mean volume lessened from postoperative day 1 after vein graft. RBC, red blood cell; FFP, fresh frozen plasma; Hb, hemoglobin; H-vac, hemovac; LMWH, low-molecular-weight heparin.
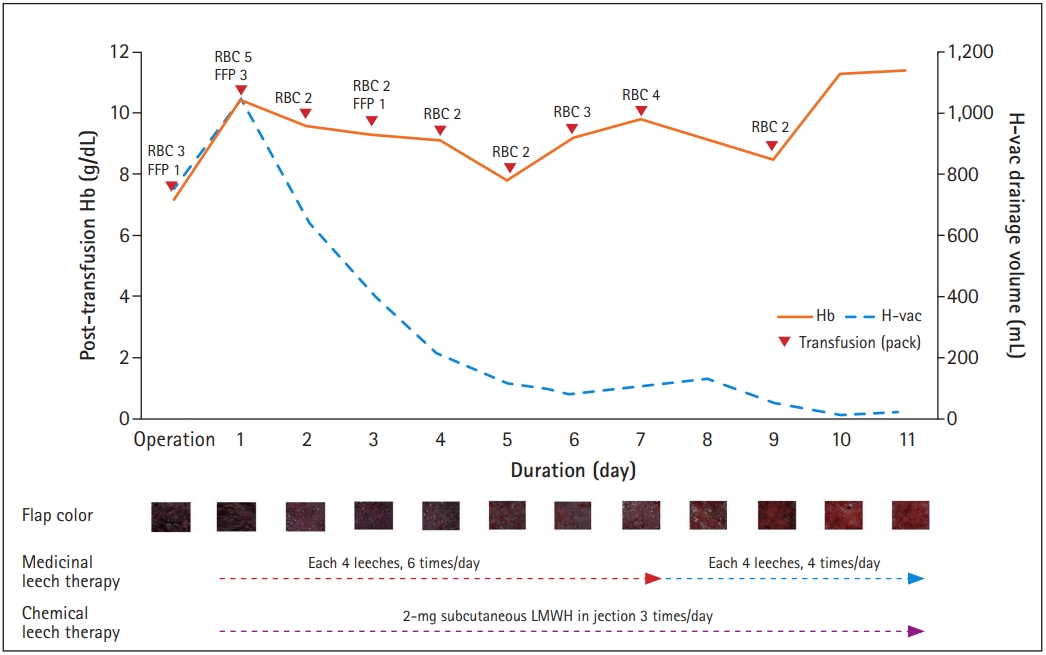
Fig. 5.
Contrast-enhanced three-dimensional computed tomographic angiography 4 months after the operation. The right (A), lateral (B), left (C) angles. On the lateral view, the right superficial temporal artery and vein are enhanced and delineated. However, the left superficial temporal artery and vein were not delineated.

REFERENCES
1. Miller GD, Anstee EJ, Snell JA. Successful replantation of an avulsed scalp by microvascular anastomoses. Plast Reconstr Surg. 1976;58:133-6.


2. Cheng K, Zhou S, Jiang K, et al. Microsurgical replantation of the avulsed scalp: report of 20 cases. Plast Reconstr Surg. 1996;97:1099-106.


3. Barisoni D, Lorenzini M, Governa M. Two cases of scalp reimplantation based on one artery and one vein with interposed vein grafts. Eur J Plast Surg. 1997;20:51-3.


4. Herrera F, Buntic R, Brooks D, Buncke G, Antony AK. Microvascular approach to scalp replantation and reconstruction: a thirty-six year experience. Microsurgery. 2012;32:591-7.


5. Ding W, Liu M, Chen L, Xu L, Rui Y, Gu Y. Treatment of total scalp avulsion by an advanced microsurgical method involving the subcutaneous tissue suspension by the tight suture of scalp tissue around anastomotic stoma. J Craniofac Surg. 2015;26:579-81.


6. Jin Y, Hua C, Hu X, et al. Microsurgical replantation of total avulsed scalp: extending the limits. J Craniofac Surg. 2017;28:670-4.


7. Nguyen HH. The microsurgical replantation of seven complete scalp avulsions: is one artery sufficient? J Plast Reconstr Aesthet Surg. 2012;65:1639-44.


8. Nguyen MQ, Crosby MA, Skoracki RJ, Hanasono MM. Outcomes of flap salvage with medicinal leech therapy. Microsurgery. 2012;32:351-7.


-
METRICS

-
- 0 Crossref
- 3,442 View
- 59 Download
- Related articles in Arch Hand Microsurg
-
Successful Replantation after Amputation around Both Knee2020 June;25(2)
Replantation for Segmental Amputation of the Digits and Hand: A Case Report2016 November;25(2)
Microsurgical Replantation of Very Distally Amputated Finger2007 November;16(2)