Painful eccrine spiradenoma containing nerve fibers in the forearm: a case report
Article information
Abstract
Eccrine spiradenomas are rare benign adnexal tumors that originate from the eccrine glands. They mainly arise in the head, neck, and upper trunk of young adults and are sometimes accompanied by pain and tenderness. Although spontaneous pain is a typical symptom of eccrine spiradenoma, the underlying mechanism remains unclear. We report the case of a patient who had a spiradenoma in the subcutaneous tissue of the left forearm that was accompanied by agonizing pain triggered by pressure. A 42-year-old man who had undergone surgical excision of a left forearm mass 5 years ago presented for relapsed pain and a palpable mass at the previous excision site. The agonizing pain had been triggered a few days ago, in response to even a slight touch. The mass measured approximately 0.8×0.8 mm, and there were no changes visible around the scar. Irregularly shaped masses, each measuring approximately 5 mm, were removed with a 2-mm safety margin from the subcutaneous fat. A histopathologic examination revealed that the resected nodules were surrounded by delicate fibrous capsules, some parts of which contained blood vessels and prominent thickened nerve fibers. By the time of the 6-month follow-up, the masses had not recurred, and the biopsy site was well maintained without pain. We describe the surgical and histopathologic findings of an isolated eccrine spiradenoma accompanied by recurrent agonizing pain. The peculiar microscopic arrangement of the thickened nerve fibers encasing the nodule of eccrine spiradenoma may correlate with its pain mechanism.
Introduction
Eccrine spiradenoma, first described in 1956 by Kersting and Helwig [1], is a dermal tumor of skin adnexa that originates from the eccrine glands. Though it is included among the nine skin tumors that can cause pain (the others being leiomyoma, neuroma, dermatofibroma, angiolipoma, neurilemmoma, endometrioma, glomus tumor, and granular cell tumor) [2], the occurrence of pain in eccrine spiradenoma is relatively rare and not a typical feature.
The most common sites are the head and neck, which account for approximately 36% of these tumors. One case was associated with head and neck malignancy [3] These tumors can also arise in the trunk and other sites. They are extremely rare; only 50 cases have been reported, accounting for approximately 1 per 13,000 specimens, especially from the hand [4]. Differential diagnosis and appropriate treatment of eccrine spiradenomas are important because they can undergo malignant transformation.
In our case, we report an uncommon presentation of eccrine spiradenoma on the forearm, where severe pain was a significant symptom. This rare presentation, potentially due to nerve fiber involvement, challenges the conventional perception of eccrine spiradenoma as typically being non-painful masses.
Case report
A 42-year-old man, who had undergone surgical excision of a mass on the left forearm 5 years ago, presented with relapsed pain and a palpable mass on the previous excision site. The patient had undergone the previous excision at other hospitals and the histologic diagnosis was unknown because biopsy was not performed. A new mass was approximately 0.8×0.8 cm in size, and no specific abnormalities were noted around the lesion (Fig. 1). Agonizing pain was triggered a few days ago, whenever the mass was touched slightly. In consideration of the lesion’s location and the patient’s symptoms, including the severe pain upon slight touch, a differential diagnosis of superficial radial nerve neuroma is indeed warranted. The proximity of the mass to the known course of the superficial radial nerve, combined with the presentation of agonizing pain, aligns with the clinical features typically associated with neuromas. Therefore, the surgical excision and subsequent histopathological examination were also intended to evaluate the possibility of a neuroma, in addition to confirming the eccrine spiradenoma.
The mass was excised through an elliptical incision under local anesthesia and the wound was closed through primary repair. The solitary irregularly shaped mass measuring approximately 5 mm was removed from the subcutaneous fat with a 2-mm margin (Fig. 2) and subjected to biopsy for accurate diagnosis and to decide further treatment plan.
Histopathologic examination revealed that the nodule was surrounded by a delicate fibrous capsule, some part of which contained blood vessels and prominent thickened nerve fibers (Fig. 3). During the two-year follow-up period post-surgery, the patient showed no signs of recurrence. This outcome is particularly significant, as eccrine spiradenomas, though generally benign, have been known to recur in some cases. The absence of recurrence in our patient over this extended period underscores the success of the surgical intervention and may provide valuable insights into the long-term management of eccrine spiradenomas.
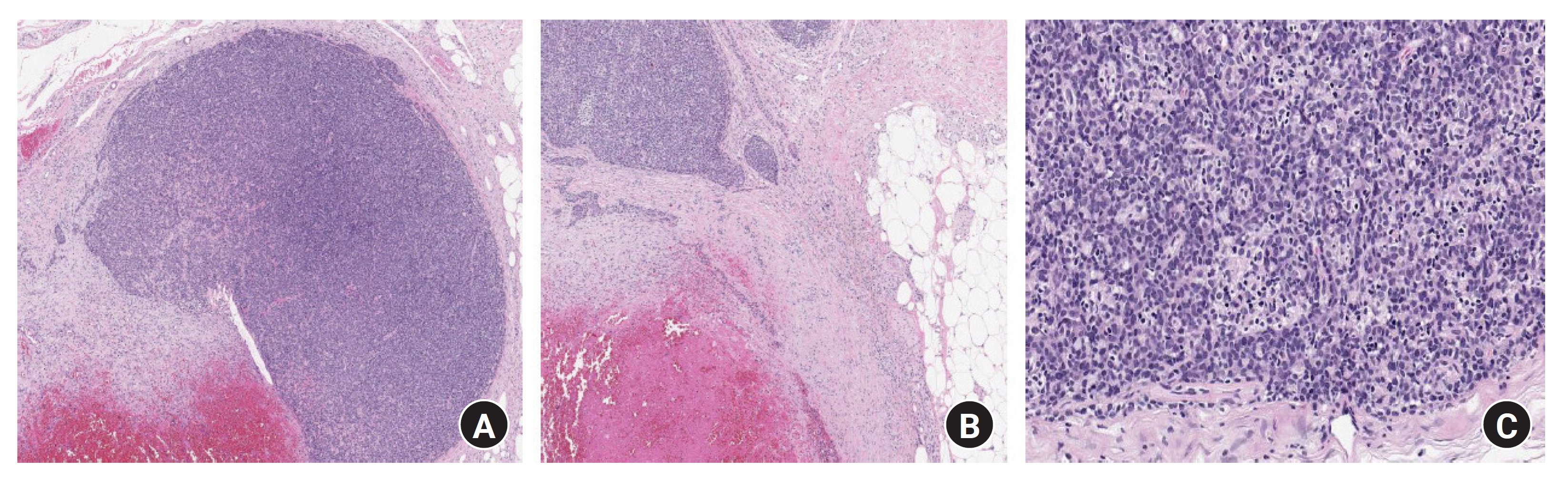
Microscopic findings (hematoxylin and eosin staining). (A) Well-circumscribed and encapsulated tumor nodule with smooth borders in the dermis and subcutaneous tissue, some of which contained blood vessels and prominent thickened nerve fibers (×40). (B) A capsule area containing nerve fibers (x40). (C) Tumor lobules composed of two cell types. Peripherally, smaller dark blue cells and centrally, pale larger cells. (x100).
Discussion
Eccrine spiradenomas can be solitary or multiple lesions. Solitary eccrine spiradenoma can arise in various parts of the body, usually in the front, and above the waistline [5]. In some cases, multiple lesions manifest in a linear or zosteriform distribution [6]. Especially it is extremely rare on the forearm. We describe the surgical and histopathological findings of an isolated eccrine spiradenoma on the forearm.
Eccrine spiradenomas are difficult to differentiate from others clinically. Histopathologic study is crucial to diagnosis. They are composed of three types of cells (epithelial cells, myoepithelial cells, and lymphocytes). Eccrine spiradenomas may be accompanied by similar tumors of apocrine origin, such as trichoblastomas, and cylindromas. Histologically, the eccrine glands have cells with relatively clear cytoplasm and occasionally contain squamous epithelium, whereas cells of the apocrine glands have eosinophilic cytoplasm and nuclei located off-center [5].
In our patient, the eccrine spiradenoma was accompanied by agonizing pain. Eccrine spiradenoma is one of nine types of skin tumors that can manifest with pain; therefore, it should be considered when a skin tumor is painful. The presence of pain or tenderness has been reported in 23% to 91% of patients with eccrine spiradenomas [1,7]. The mechanism of pain is not completely clear, but the peculiar microscopic arrangement of the thickened nerve fibers surrounding the nodules of eccrine spiradenoma may be involved [8]; pain is thought to be generated when small unmyelinated axons penetrate the hyalinized stromal mantle [9]. Other investigators have suggested that the expansion of cysts in the tumor is also involved with pain [10].
Eccrine spiradenoma rarely undergoes malignant transformation. Such a change may occur if the tumor has been present for a long time, and it is clinically manifested by rapid enlargement of the cystic component. Malignant transformation of eccrine spiradenomas shares many clinical and pathologic features with that of dermal cylindromas. The carcinomas that develop from eccrine spiradenomas often retain architectural features evocative of cylindroma, including a pattern of closely spaced cellular nests and trabeculae, a basaloid cell type, and remnants of hyaline membranes about some tumor nests [7]. While the exact etiology of eccrine spiradenoma remains unclear, several predisposing factors have been proposed in the literature. Genetic predisposition is considered one of the potential contributing factors. Studies have shown that mutations in the CYLD gene, which is also associated with other skin adnexal tumors like cylindromas and trichoblastomas, may play a role in the development of eccrine spiradenomas. This mutation leads to the disruption of normal cell cycle regulation and tumor suppression pathways. Environmental factors may also contribute to the development of these tumors. Continuous skin irritation or trauma has been suggested as a possible triggering factor, especially in cases where eccrine spiradenomas arise in atypical locations, such as the forearm, as in our patient. Additionally, hormonal influences are speculated to play a role, given the observation that eccrine spiradenomas can change in size and symptomatology during pregnancy or hormonal therapy. However, more research is needed to establish a definitive link between hormonal changes and the development of these tumors. In summary, while the pathogenesis of eccrine spiradenoma is not fully understood, genetic factors, environmental triggers, and hormonal influences are considered potential predisposing factors. Understanding these factors may provide insights into more effective prevention and treatment strategies.
Eccrine spiradenomas rarely arise in the forearm. When they are accompanied by neurologic symptoms, such as pain, they can be misdiagnosed as neuromas, neurilemmomas, or others of the nine pain-causing skin tumors [2,4]. In addition, nerve involvement may induce pain, and malignant transformation, although rare, is possible. Therefore, skin tumors that cause pain should be resected completely, and their histopathologic features should be verified. Regular follow-up observations for the recurrence of this tumor are also necessary. Eccrine spiradenoma should be distinguished from other skin tumors, and a treatment plan, devised on the basis of other case reports, should be established.
Notes
The authors have nothing to disclose.
Funding
None.


