|
 |
- Search
| Arch Hand Microsurg > Volume 29(1); 2024 > Article |
|
Abstract
Purpose
This retrospective study aimed to identify factors influencing hand flexor tendon rerupture and to develop preventive strategies for patients who have undergone hand flexor tendon repair.
Methods
In total, 287 patients who underwent hand flexor tendon repair between January 2011 and June 2022 were included. Patients with thumb injuries, amputations, bone injuries, extensor tendon injuries, and those with less than 3 months of follow-up were excluded. Patients were divided into rerupture and non-rerupture groups. Events leading to ruptures were also investigated. The two groups were compared according to sex, age, occupation, smoking status, history of diabetes mellitus, injury characteristics, core suture method, and timing of the rehabilitation course.
Results
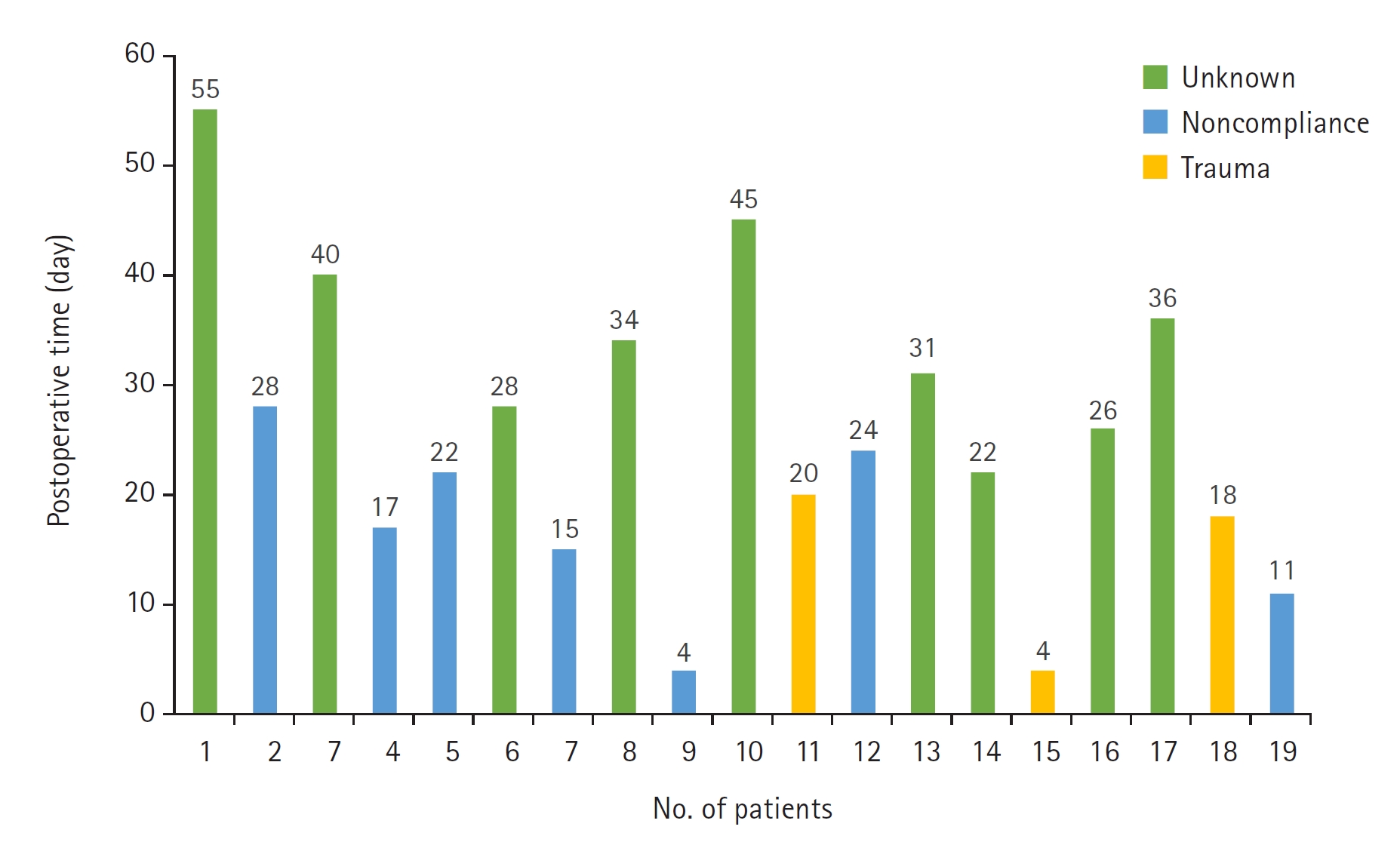
Of the 287 patients, 19 experienced rerupture (6.6%). The mean time to rerupture was 25.3 days. Reruptures occurred due to unknown causes in nine cases (47.4%), noncompliance with medical recommendations in seven cases (36.8%), and trauma in three cases (15.8%). Among the investigated factors, little finger injury and concurrent flexor digitorum superficialis (FDS) and flexor digitorum profundus (FDP) ruptures were significantly associated with rerupture. Little difference was noted in the core suture methods and timing of the rehabilitation course between the two groups.
Conclusion
To minimize the risk of rerupture, patients should strictly adhere to medical recommendations and avoid any activities that could cause trauma for at least 1 month after surgery, which is the critical period for tendon remodeling. Patients with little finger injuries as well as concurrent FDS and FDP ruptures require special attention and careful monitoring.
Flexor tendon injuries often occur in young working individuals as well as impose a significant burden on society. Loss of flexion can limit activities of daily living and hinder work-related tool use [1]. Surgical techniques, materials, and rehabilitation protocols for flexor tendon repair have been developed over several decades, thus increasing success rates while decreasing complication rates [2]. Major complications associated with this type of injury are tendon adhesion and rupture. Tendon rerupture is a serious complication that completely inhibits flexion, thus necessitating reoperation. The reported rerupture rates vary between 4% [1] and 11% [3].
Although flexor tendon injuries are common, few studies have examined the causes and risk factors of rerupture. In this retrospective study, we investigated cases involving rerupture and their incidence following hand flexor tendon repair using data from our clinic. This study aimed to identify the factors influencing rerupture and to develop preventive strategies for patients who underwent flexor tendon repair. We hypothesized that certain factors or preexisting conditions significantly impact the need for rerupture and that addressing these factors would significantly decrease the incidence of rerupture.
Ethics statement: This study was performed in accordance with the Declaration of Helsinki. Written informed consent was obtained from the patients for the publication of this study including all clinical images. The study design was approved by the Institutional Review Board of Gwangmyeong Sungae General Hospital (No. KIRB-2023-N-008).
We retrospectively reviewed the medical records of patients who underwent hand flexor tendon surgery at our clinic between January 2011 and June 2022. The exclusion criteria included the following: thumb injuries, amputations, bone injuries, extensor tendon injuries, and follow-up periods less than 3 months. Patients were divided into rerupture and non-rerupture groups. In the rerupture group, we investigated rerupture events and their specific date of occurrence.
We investigated various potential factors influencing postoperative rupture, including patient, injury, surgical, and rehabilitation factors. Patient factors included age at injury, sex, diabetes mellitus, occupation, and smoking status, with occupations further classified as blue-collar, white-collar, or non-employed. Injury factors included injury characteristics, work relations, injured fingers, tendons, and zones. Injury characteristics were further categorized as damage caused by metal blades, glass, other sharp objects, and blunt or crushing forces. Surgical factors included the core suture technique and the number of core strands used for repair. In our clinic, the modified loop suture and modified Kessler method are commonly used, with core strands ranging from two to eight. All the ruptured flexor tendons were repaired using absorbable polydioxanone sutures. To prevent adhesions, our rehabilitation protocol involved initiating self-exercise with passive flexion and careful early active mobilization within the splint from the time when the bleeding stopped after surgery. Subsequently, physical therapy was administered by a skilled therapist for a full passive range of movement. Once the tendon had matured during the healing process, the splint was removed; a full active range of flexion movement was encouraged. However, the timing of each step in the rehabilitation process was determined on a case-by-case basis according to the physician’s judgment based on the wound condition. Therefore, the rehabilitation factors included the number of postoperative days until physical therapy was initiated and the number of days until splint removal.
Descriptive statistics, such as mean, standard deviation, range, number, and percentage, were used to report the factors. Nominal variables between groups were compared using the chi-square or Fisher exact tests, as appropriate, for data size and distribution. Continuous variables were analyzed using the Student t-test when following a normal distribution, or with the Mann-Whitney U-test if otherwise. Logistic regression analysis was performed to evaluate the variables related to rerupture, as selected in the univariate analysis. For two or more independent variables, multinomial logistic regression analysis was used to simultaneously identify their influence and direction to determine causal relationships. Statistical significance was set at a p-value of <0.05. Data analysis was conducted using IBM SPSS Statistics for Windows, ver. 26.0 (released in 2019 by IBM Corp., Armonk, NY, USA).
Between 2011 and 2022, 287 patients with flexor tendon rupture were included in the study, of whom 19 (6.6%) experienced rerupture. In the rerupture group, seven patients (36.8%) experienced rerupture due to noncompliance with medical recommendations, three (15.8%) due to trauma, and nine (47.4%) had no clear cause (Table 1). Reruptures occurred between days 4 and 56 after the initial surgery, with an average of 25.3 days. All 19 patients underwent successful revision surgery without complications, such as further ruptures or significantly limited range of motion; Figs. 1 and 2 show cases of revision surgery in patients with rerupture. The comparison results of the non-rerupture (n=268) and rerupture (n=19) groups according to different factors are presented below.
The average age in the rerupture group was 43.6 years, as compared to 40.4 years in the non-rerupture group. Blue-collar workers comprised the largest occupation group in both groups. The rerupture group included a higher percentage of smokers (47.4%) than the non-rerupture group (32.8%). Additionally, more patients had a history of diabetes mellitus in the rerupture group (15.8%) than in the non-rerupture group (6.3%). However, these differences were not statistically significant.
The index finger was the most frequently injured, accounting for 108 patients (37.6%), followed by the little finger (68 patients, 23.7%). This trend was also observed in the non-rerupture group. However, in the rerupture group, the little finger was the most injured in nine patients (47.4%); this result was statistically significant, indicating an association between the injured finger and rerupture (p=0.032) (Table 2). In both groups, flexor tendon rupture occurred most frequently in zone 2, with knife damage being the most common cause. Three types of injuries were observed: flexor digitorum superficialis (FDS) rupture, flexor digitorum profundus (FDP) rupture, and concurrent FDS and FDP ruptures. In the non-rerupture group, FDP rupture was the most common type of injury in 164 patients (61.2%), whereas concurrent FDS and FDP ruptures were the most common types of injury in 11 patients (57.9%). Conversely, in the non-rerupture group, concurrent FDS and FDP ruptures ranked second with 67 patients (25.0%). This factor was significantly associated with rerupture of the injured finger (p=0.013) (Table 2).
Both groups most frequently used the modified Kessler technique and the 4-strand core method, with no significant statistical difference (Table 2). In the rerupture group, some patients experienced ruptures before being advised to start physical therapy or to remove their splints. These instances were excluded from the statistical analysis (Table 1). The average number of postoperative days until physical therapy was 7.2 days for the non-rerupture group and 7.0 days for the rerupture group. The average number of postoperative days until splint removal was 24.1 days for the non-rerupture group and 22.9 days for the rerupture group. There were no significant differences in the timing of the rehabilitation process between the two groups (Table 2).
In the univariate analysis, little finger injury and concurrent FDS and FDP tendon ruptures showed significant differences between the two groups. A multivariate logistic regression analysis was conducted focusing on the two selected independent variables. The reference for each analysis was set as index finger injury and FDP tendon rupture, which represented the highest proportion of their respective variables among all patients. The odds ratio for concurrent FDS and FDP tendon rupture was 2.144 (p=0.032), indicating a 2.144-times higher risk of rerupture than in cases with only FDP tendon rupture (Table 3). In addition, little finger injury had an odds ratio of 2.789 (p=0.008), thus suggesting a 2.789-times higher risk of rerupture than index finger injury (Table 3).
Despite advancements in surgical techniques and rehabilitation methods, flexor tendon rerupture remains a difficult complication to predict. It is thus challenging to accurately determine the cause of rerupture, particularly when flexion force was not observed during the postoperative follow-up after tendon repair. Even direct examination of the ruptured tendon during reoperation may not provide a precise understanding of the specific mechanism behind the rupture. Therefore, referencing previous studies and identifying predictable risk factors are important for reducing the uncertainty in predicting reruptures and achieving better outcomes after tendon repair.
Among the rerupture events, 36.8% (7 of 19 patients) occurred when patients removed their splints early and engaged in activities against medical advice, such as returning to work or lifting heavy objects. Moreover, 15.8% (three patients) experienced rerupture due to direct trauma, such as falling or hitting an object. Harris et al. [4] reported that approximately half of the patients experienced reruptures due to imprudent postoperative behavior or activities involving excessive force despite warnings. This suggests that patient behavioral patterns are closely linked to rerupture. Often, patients overlook medical advice, think that their surgery site will be fine, and participate in strenuous activities that can render the surgery futile and necessitate revision. In cases with unknown causes accounting for 47.4% of cases (nine patients), some reported an inability to move their fingers upon waking or rerupture during normal self-mobilization. This is supported by the observation that there were no instances of a third rerupture, likely because the patients became more cautious and adhered to recommendations following reoperation.
The average time to rerupture was 25.3 days, with patterns dependent on preceding events. Reruptures due to noncompliance or trauma usually occurred within a month, whereas those of unknown etiology tended to occur later (Fig. 3). One month marks the transition in the tendon healing stages from inflammation and proliferation to the initial phase of remodeling [5]. During this phase, tight connections are formed between the tendon ends; collagen fibers begin to orient longitudinally along the tendon axis [6]. The tendons were more vulnerable before this phase. Therefore, education and careful monitoring to prevent noncompliant behaviors are crucial, at least for the first month.
Little finger injuries are known to have difficulty achieving good outcomes after primary repair of the flexor tendon [7]. Gault [8] reported that surgery in zone 2 resulted in less satisfactory outcomes in the little finger than in other fingers. Dowd et al. [9] investigated the rate of rerupture after tendon repair in zones 1 and 2 and found that the little finger had a significantly higher rate of rerupture than the other fingers. Elliot and Giesen [10] reported a 35% chance of hindrance to grip function and a 20% chance of a second rupture in the little finger after primary tendon repair, which was exclusively a problem for the little finger. Of the 287 cases, 63 involved the little finger; among them, 8 (12.7%) were reruptured, which is much higher than the overall rerupture rate of 6.6%. Although previous studies have shown consistency with our results, they did not formally establish little finger injury as a statistical risk factor for rerupture. However, we used logistic regression analysis to explicitly demonstrate that injury to the little finger was a statistically significant and predictable risk factor for rerupture.
The little finger naturally rests in a more flexed position than the other fingers; its flexor mechanism is stronger than that of the extensors [8]. To restore a stronger flexor mechanism, greater tensile strength is required for normal function. This suggests that tendon healing in the little finger may require a longer duration to stabilize than in the other fingers. The little finger is particularly vulnerable to injury because it is the outermost digit apart from the thumb. In the gripping position, it is subjected to a greater force than the other fingers; the significant angle of flexion under this force may increase the risk of rerupture. Additionally, owing to the small size of the finger and consequently the smaller tendon sheath, it may not adequately support the bulge of the repair [8,11]. These features can negatively affect tendon maturation and rehabilitation following primary repair, thus increasing the likelihood of complications such as adhesions and reruptures.
The most common type of tendon injury in our study was an isolated rupture of the FDP. However, we observed a significant increase in concurrent FDS and FDP ruptures in patients who experienced rerupture. This concurrent injury was identified as a predictable risk factor for rerupture, as confirmed by the chi-square and logistic regression analyses. Similar findings were reported by Svingen et al. [12], who also noted a link between concurrent FDS and FDP ruptures and the likelihood of rerupture. Simultaneous rupture of both tendons indicated severe damage, thus leading to greater disruption of adjacent physiological structures than a single tendon rupture. In our study, this occurred exclusively in zone 2, an area where the tendons are tightly encased within a narrow sheath and accompanied by pulleys as well as aponeurotic structures that facilitate their movement and alignment. When an injury occurs in this area, the resulting development of inflammatory granulation tissue hinders tendon healing; damage to surrounding tissues may negatively affect the essential nutritional supply needed for tendon repair [13]. Therefore, the extensive damage caused by the rupture of both tendons makes it difficult to prevent rerupture. In addition, the rupture of both tendons, as opposed to only one, resulted in a more substantial loss in tensile strength. This weakened support may increase the risk of rerupture; it takes time for both tendons to regain sufficient tensile strength to support the load effectively.
The modified Kessler method is commonly used for flexor tendon repair [14,15]. In addition, we frequently use the loop suture technique in our practice. This technique involves passing another suture through a loop created by the initial suture, which holds the tendon ends together while providing sufficient tensile strength [16]. In our study, of the 223 cases employing the modified Kessler method, 17 (7.6%) experienced rerupture. In contrast, with the loop suture technique, only two of the 57 patients (3.5%) experienced rerupture. Lee [17] conducted experiments on human tendons and found that the double-locking loop suture displayed greater tensile strength than the Kessler method. Specifically, 1/3 of the Kessler group exhibited a gap of 3 to 5 mm, in contrast to almost none in the double-loop locking suture group. These findings suggest that the loop suture technique is as effective as the modified Kessler method in providing adequate tendon strength and that the choice of suture method is not a significant risk factor for rerupture, as supported by statistical analysis.
The four-strand core suture is the most frequently used among two-, four-, six-, and eight-strand core sutures [14]. Although tendon strength increases with the number of core strands [17], a low number of strands in the initial tendon repair was not a risk factor for rerupture. Various factors, such as core suture purchase, suture anchor size, curvature of tendon gliding, and the presence of an intact major pulley also contribute to strength; therefore, the number of core strands alone cannot be the sole basis for judgment [18]. Furthermore, research suggests that a higher number of core strands is not inherently superior to a lower number of strands [19]. According to that study, a higher number of strands may increase resistance to movement, which could ultimately increase the risk of rupture [20]. Surgeons must consider the time and complexity of the surgical procedure when selecting an appropriate number of core strands for tendon repair. It is helpful to keep in mind that a small number of core strands do not necessarily increase the risk of rerupture, thus aiding surgeons in making informed decisions.
Rehabilitation strategies for hand flexor tendon repair have changed over the years. Initially dominated by passive motion protocols, early active motion was adopted. This shift occurred because active movement promoted better tendon glide and excursion [21]. Despite concerns that active motion might increase the risk of rerupture, its functional benefits outweigh this risk [22]. In our study, we used a consistent protocol that induced both early passive and active mobilization. Our investigation focused on whether the timing of initiating full active and passive ranges of movement influenced rerupture rates. The results indicated that the timing of these exercises was not significantly correlated with the risk of rerupture.
The limitations of this study include the reliance on patient reports to document rerupture events, which makes verifying their accuracy challenging. The comparison of surgical techniques was confined to the modified Kessler method and the loop suture technique employed in our institution, without considering other surgical methods. In terms of rehabilitation, the comparison was limited to the timing of our protocol, which lacked a broader comparison of different protocols. As a single-center study, there is a limitation in the sample size, which could be addressed by multicenter research to potentially enhance statistical objectivity and accuracy. Furthermore, the retrospective nature of the study and the involvement of human scoring could introduce errors or biases, even when using objective assessment tools.
Flexor tendon rerupture often occurs because of patient negligence or disregard of postoperative recommendations, typically within the first month after surgery. Therefore, it is essential to provide thorough patient education and to emphasize the importance of adherence to the guidelines during this critical period. The risk of rerupture is particularly high in patients with little finger injuries or concurrent FDS and FDP ruptures. Because these factors are determined at the time of injury and cannot be modified, they should be used to identify patients requiring careful monitoring and management.
Fig. 1.
A 16-year-old girl presented with a complete rupture of the flexor digitorum profundus (FDP) tendon due to a cutter knife injury. (A, B) Intraoperative images from the initial repair of the FDP tendon. (C) A 28-day follow-up image showing flexion failure of the distal interphalangeal joint after throwing a book. (D, E) Intraoperative images from the re-repair of the FDP tendon. (F) An 8-month follow-up image after reoperation showing a full range of active flexion motion.
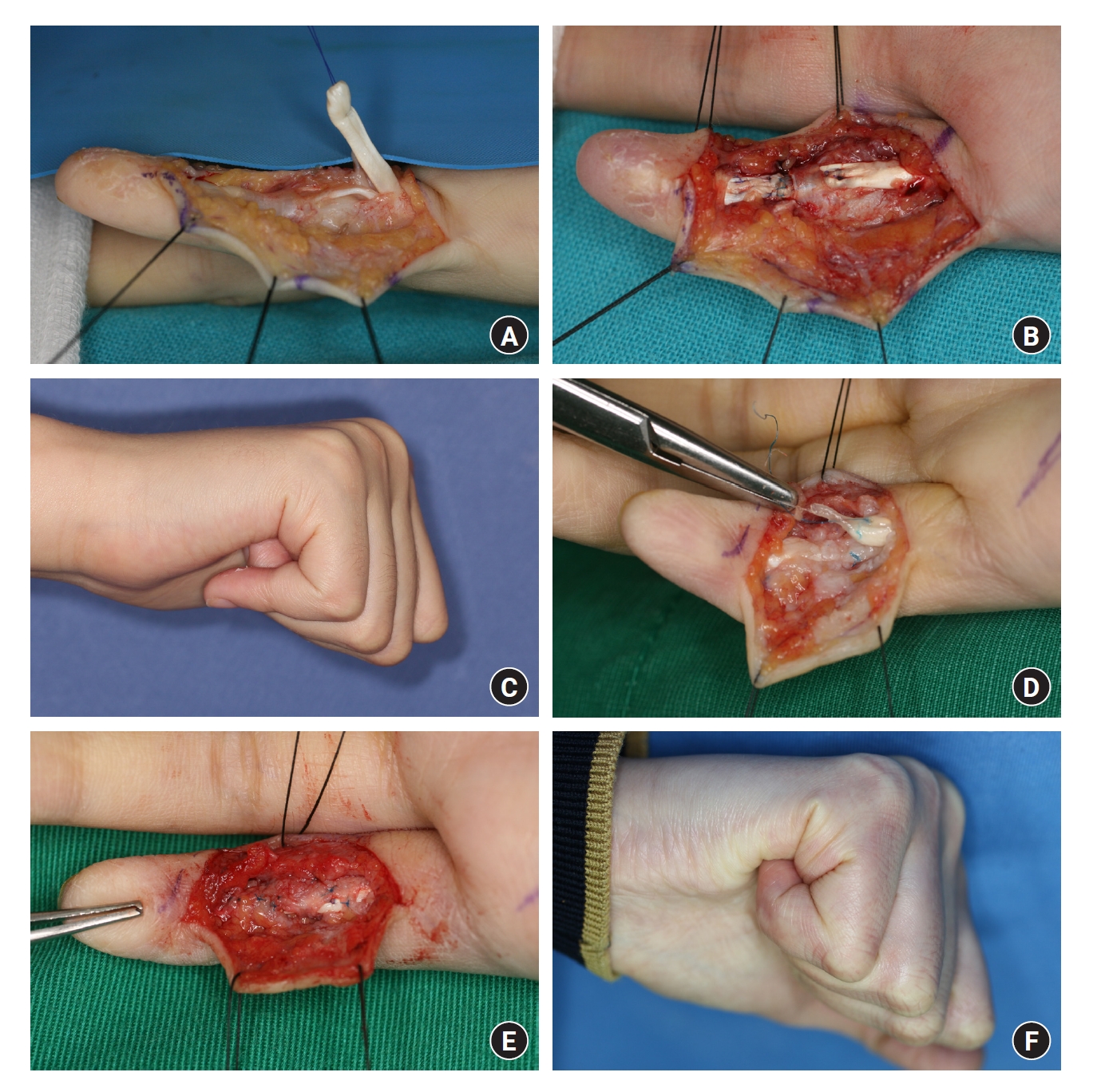
Fig. 2.
A 62-year-old man presented with a complete rupture of the flexor digitorum superficialis (FDS) and flexor digitorum profundus (FDP) tendon due to an injury from broken glass. (A, B) Intraoperative images from the initial repair of the FDS and FDP tendons. (C) A 36-day follow-up image showing a limited range of active flexion motion after grabbing a cellphone. (D, E) Intraoperative images from the re-repair of the FDP tendon, with the intact FDS tendon. (F) A 10-month follow-up image after reoperation showing improvement in the range of active flexion motion.
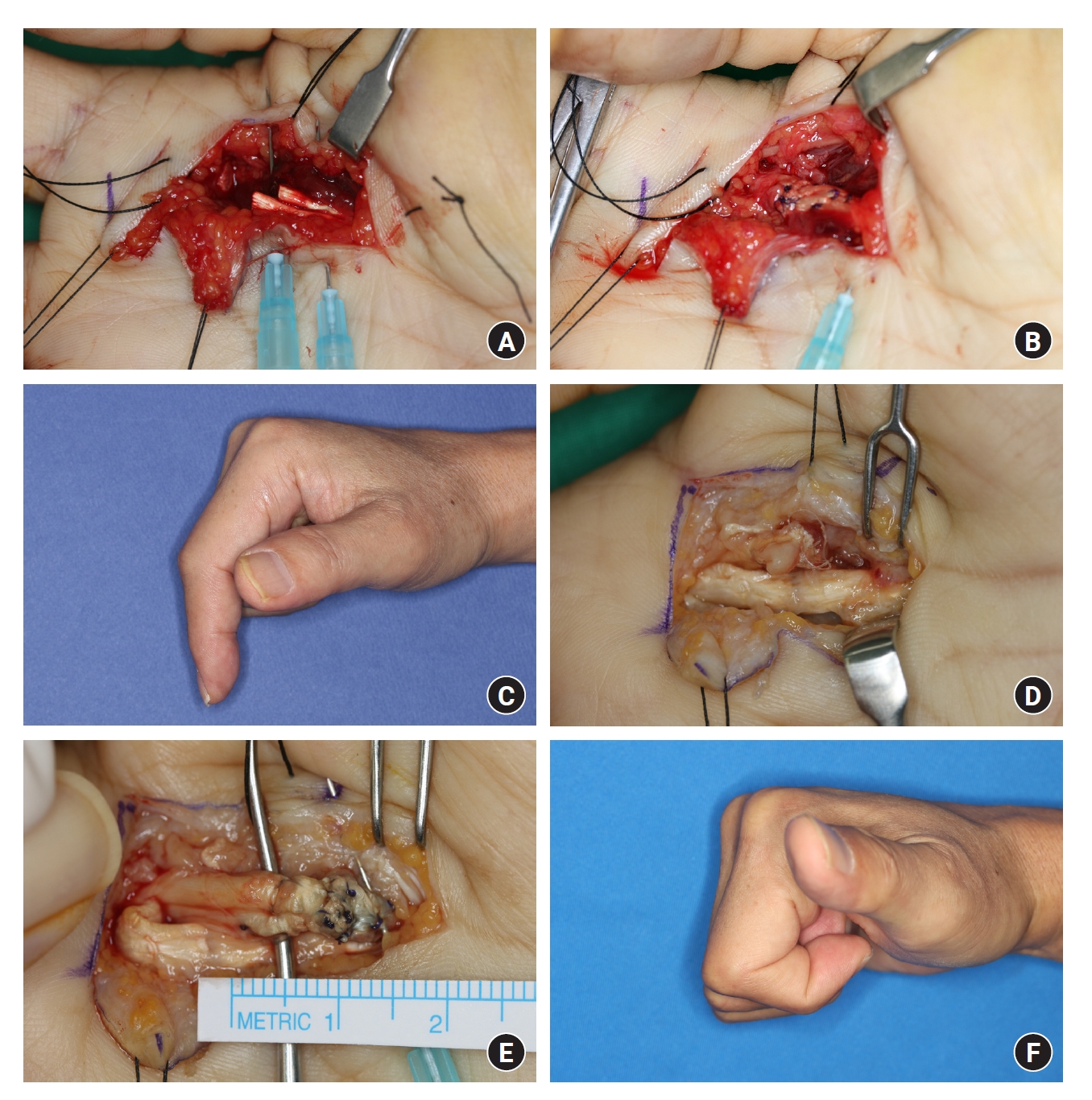
Table 1.
Patient information for the rerupture group (n=19)
Table 2.
Comparative analysis of sociodemographic and injury characteristics, suture methods, and rehabilitation
Table 3.
Multivariable logistic regression analysis to identify the predictive factors for rerupture
| Independent variable | Beta | SE | Exp(β) | P-value |
|---|---|---|---|---|
| Finger | ||||
| Index | Reference | Reference | Reference | |
| Middle | 0.290 | 0.503 | 1.336 | 0.567 |
| Ring | 0.546 | 0.571 | 1.728 | 0.318 |
| Little | 0.026 | 0.503 | 2.789 | 0.008* |
| Tendon | ||||
| FDS | –0.518 | 0.564 | –0.919 | 0.358 |
| FDP | Reference | Reference | Reference | |
| Both | 1.241 | 0.578 | 2.144 | 0.032* |
References
1. Dy CJ, Daluiski A, Do HT, Hernandez-Soria A, Marx R, Lyman S. The epidemiology of reoperation after flexor tendon repair. J Hand Surg Am. 2012;37:919-24.


2. Dy CJ, Hernandez-Soria A, Ma Y, Roberts TR, Daluiski A. Complications after flexor tendon repair: a systematic review and meta-analysis. J Hand Surg Am. 2012;37:543-51.


3. Ibrahim MS, Khan MA, Rostom M, Platt A. Rupture rate following primary flexor tendon repair of the hand with potential contributing risk factors. Surg Technol Int. 2014;24:363-7.

4. Harris SB, Harris D, Foster AJ, Elliot D. The aetiology of acute rupture of flexor tendon repairs in zones 1 and 2 of the fingers during early mobilization. J Hand Surg Br. 1999;24:275-80.



5. Gomez M. The physiology and biochemistry of soft tissue healing. In: Griffin L, editor. Rehabilitation of the injured knee. St. Louis, MO: Mosby; p. 34-44.
6. Lin TW, Cardenas L, Soslowsky LJ. Biomechanics of tendon injury and repair. J Biomech. 2004;37:865-77.


7. Rigo IZ, Røkkum M. Predictors of outcome after primary flexor tendon repair in zone 1, 2 and 3. J Hand Surg Eur Vol. 2016;41:793-801.



9. Dowd MB, Figus A, Harris SB, Southgate CM, Foster AJ, Elliot D. The results of immediate re-repair of zone 1 and 2 primary flexor tendon repairs which rupture. J Hand Surg Br. 2006;31:507-13.



10. Elliot D, Giesen T. Primary flexor tendon surgery: the search for a perfect result. Hand Clin. 2013;29:191-206.


11. Orkar KS, Watts C, Iwuagwu FC. A comparative analysis of the outcome of flexor tendon repair in the index and little fingers: does the little finger fare worse? J Hand Surg Eur Vol. 2012;37:20-6.



12. Svingen J, Wiig M, Turesson C, Farnebo S, Arner M. Risk factors for reoperation after flexor tendon repair: a registry study. J Hand Surg Eur Vol. 2022;47:1071-6.




13. Jia Q, Chen D, Guo J, et al. Risk factors associated with tendon adhesions after hand tendon repair. Front Surg. 2023;10:1121892.



14. Wongsiri S, Liawrungrueang W. Biomechanical study of a newly developed continuous double knots technique compared with the 4-strand double-modified Kessler technique for flexor tendon repair. J Exp Orthop. 2021;8(1):79.




15. Berezin PA, Zolotov AS, Volykhin RD, Evdokimova EN, Morozov LI, Lazarev IA. Rozov and Kessler tendon sutures: common properties and differences. Traumatol Orthop Russ. 2022;28:167-75.


16. Lee KC, Lee DC, Kim JS, Ki SH, Roh SY, Yang JW. Loop suture technique for flexor digitorum profundus tendon repair in the insertion site. J Korean Soc Plast Reconstr Surg. 2010;37:650-8.
17. Lee H. Double loop locking suture: a technique of tendon repair for early active mobilization. Part I: Evolution of technique and experimental study. J Hand Surg Am. 1990;15:945-52.


18. Winters SC, Seiler JG 3rd, Woo SL, Gelberman RH. Suture methods for flexor tendon repair: a biomechanical analysis during the first six weeks following repair. Ann Chir Main Memb Super. 1997;16:229-34.


19. Shaharan S, Bage T, Ibrahim N, Diamantopoulos A, Doswell K, Dheansa B. Rupture rates between 2-strand and 4-strand flexor tendon repairs: is less more? Ann Plast Surg. 2020;84:43-6.


20. Dogramaci Y, Kalaci A, Sevinç TT, Esen E, Komurcu M, Yanat AN. Does strand configuration and number of purchase points affect the biomechanical behavior of a tendon repair?: a biomechanical evaluation using different kessler methods of flexor tendon repair. Hand (N Y). 2008;3:266-70.