|
 |
- Search
| Arch Hand Microsurg > Volume 27(3); 2022 > Article |
|
Abstract
Purpose
This study compared screw and Kirschner-wire (K-wire) fixation for intra-articular fractures of the proximal phalanx head regarding the success of union and functional outcomes.
Methods
In this retrospective study, we enrolled patients with closed intra-articular fractures of the proximal phalangeal head treated between January 2011 and December 2021. Patients with open wounds, tendon or neurovascular injuries, comminuted fractures, or middle phalangeal fractures were excluded. Patients’ demographics, bone union, proximal interphalangeal (PIP) joint range of motion (ROM), grip power, and complications were collected and analyzed. The percentage of intra-articular surface involvement and the number of bone fragments were also analyzed in relation to the functional results.
Results
Among 41 patients, 21 were managed with screw fixation, and the remaining 20 with K-wire fixation. The mean union rate was 100% in the screw fixation group and 95.0% in the K-wire fixation group, with no statistically significant difference (p=0.488). Other functional parameters (PIP joint ROM, time to bone union, and grip power) were not significantly different between the two groups. Regardless of the treatment modality, the PIP joint ROM showed significant negative associations with the involvement of more intra-articular surfaces (p<0.001) and the presence of a greater number of bone fragments (p=0.040).
Conclusion
In intra-articular fractures of the proximal phalanx head, the treatment modality (screw or K-wire) did not affect the treatment outcome. Instead, the percentage of intra-articular surface involvement and the number of bone fragments showed significant negative associations with the PIP joint ROM after treatment.
Proximal interphalangeal (PIP) joint fracture of the hand occurs in nearly 0.1% of the normal population. This type of injury accounts for 0.2% to 3% of patients visiting the emergency unit and 12% to 46% of all hand fractures [1]. Usually, younger patients are injured during sports activities, middle-aged patients are injured in manual labor, and elderly patients are most commonly injured when falling down [2].
The PIP joint is a hinge joint that can extend toward the palmar side at large angles, which facilitates its large range of motion (ROM). Thus, damage may cause significant functional loss of hand [3]. Treatments are divided into two categories: conservative and surgical. Screw fixation and Kirschner-wire (K-wire) fixation are the most common options for surgery [4]. K-wire may be preferred because of the small size of the finger bone, high mobility demands, proximity of gliding structures, and small soft tissue envelope of the digits. Conversely, some studies have shown the superiority of screws due to the stronger compression force, lack of protrusion, and no need for implant removal [5].
Several studies have reported the advantages and disadvantages of screw and K-wire fixation, but few have directly compared the two treatments in terms of bone union, functional outcome, or complications. A few studies have attempted to make a comparison, but these were limited by the small or heterogeneous patient cohorts, including both proximal phalangeal head and middle phalangeal base fractures [6,7]. Since the middle phalanx and proximal phalanx have distinct mechanisms of injury [4], we believe it is difficult to draw clinically meaningful conclusions by analyzing heterogeneous types of fractures. Therefore, in this study, we directly compared screw and K-wire fixation in a homogenous group of 41 patients with closed intra-articular fractures of the proximal phalanx head.
Ethics statement: Written informed consent was obtained for publication for this study and accompanying images, and the study design was approved by the Institutional Review Board of Gwangmyeong Sungae General Hospital (No. KIRB-2022-N-003).
This retrospective study was performed on 41 patients diagnosed with closed intra-articular fractures of the proximal phalanx head of the hand and treated with screw or K-wire fixation between January 2011 and December 2021 (Table 1). The exclusion criteria were patients with extra-articular fractures, fractures in the thumb, comminuted fractures, or open fractures with soft tissue injury. Middle phalangeal base fractures were excluded because of the homogeneity of the patient group, which shares the same mechanism of injury [4]. Comminuted intra-articular fractures were excluded as such cases are not good candidates for K-wire or screw fixation [5,8]. Finally, open fractures were excluded because injuries to the ligaments and tendons surrounding the finger joint may significantly influence functional outcomes [2]. In order to rule out injuries to the collateral ligaments, we conducted physical examinations such as lateral stress tests before surgery [9].
Clinical data collected included patient demographic data, mechanism of injury, location of injury, fracture type, intra-articular surface involvement, number of bone fragments, hospital day, follow-up period, physical therapy, bone union, time for union, PIP joint ROM, grip power, secondary operation, and complications. Fracture type was classified into three categories based on radiographic data: oblique (condylar), long oblique (spiral), and longitudinal. Bone union was determined by bridging callus formation and a visible fracture line of <1 mm on plain radiography. The complications assessed were mainly sensory changes (numbness) and infection (i.e., osteomyelitis). Finally, intra-articular involvement was evaluated using plain radiography and three-dimensional reconstruction computed tomography. Based on the radiographic images, we measured the diameter (mm) and width (mm) of the total articular surface (mm2) and the largest bone fragment displaced. We then calculated the percentage of the surface area that the bone fragments occupy among the entire articular surface. The formula for intra-articular surface involvement is as followed: [diameter (mm)×width (mm) of the dominant bone fragment]/[diameter (mm)×width (mm) of the entire articular surface]×100 (%) (Fig. 1).
Statistical analysis was performed using the Student t-test, Mann-Whitney U-test, and Spearman correlation coefficients for continuous variables and the chi-square test for categorical variables. Statistical significance was set at p<0.05.
A total of 41 patients with closed intra-articular proximal phalangeal head fractures were managed in our clinic between 2011 and 2021. In total, 21 patients underwent screw fixation, and the other 20 underwent K-wire fixation. The mean ages of patients in the screw and K-wire groups were 32.6 and 27.5 years old, and the mean times to surgery were 4.6 and 3.3 days, respectively. The follow-up periods for each group were 25.9 and 13.3 weeks, respectively. Regarding the mechanism of injury, accidents during manual work (33.3%) were the main cause in the screw group, while sports activity (45.0%) was the most common cause in the K-wire group (Table 2).
Long oblique fractures were the most common (57.1%) in the screw fixation group, whereas oblique (condylar) fractures were the most common (55.0%) in the K-wire fixation group. The PIP joint intra-articular surface involvement was 51.9% in the screw fixation group and 56.5% in the K-wire fixation group. The average number of fractured bone fragments was 1.3 in the screw fixation group and 1.4 in the K-wire group (Table 2).
Under brachial plexus anesthesia, manual reduction of the fracture site was performed using C-arm imaging, followed by K-wire or screw fixation. K-wires used for fixation ranged from 0.9 to 1.1 mm in diameters. The screw used for fixation was 7 to 14 mm in length and 1.3 to 2.0 mm in thread diameter (Osteonic Inc., Seoul, Republic of Korea) (Figs. 2, 3 show the examples of successful bone union in each patient group). The number of K-wires used for fixation ranged from 1 to 3 (2.1 in average), and 1 or 2 screws were used (1.38 in average) for fixation (Tables 1, 2). An intrinsic plus-positioned short arm splint was applied postoperatively and then replaced with finger splints in the 2nd week after surgery.
To initiate early mobilization, we encouraged the patients to perform gentle active and passive exercises as soon as the swelling and pain subsided. The range of joint motion during exercise was gradually extended daily. The K-wires were removed at the outpatient clinic from week 4 to 6. For patients who underwent screw removal, an additional operation was planned on average on the 33.3rd week.
All 21 cases of screw fixation achieved radiologic union, but one out of 20 patients from the K-wire group showed nonunion at the 4th month, which Jupiter et al. [10] stated as appropriate time for judging bone union. The nonunion case in the K-wire group underwent revision surgery with screw fixation and finally reached union at the end of the follow-up period. However, the union incidence did not show a statistical difference between the two groups (p=0.488). The time for bone union for screw fixation was 7.8 weeks, which was longer than 6.8 weeks for the K-wire group. This difference between the groups was not statistically significant (p=0.123) (Table 3).
We measured the PIP joint ROM at the outpatient clinic. The mean PIP joint ROM in the screw group was 66.4° at an average of 25.9 weeks postoperatively, which was larger than the 64.0° in the K-wire group at an average 13.3-week follow-up. However, this difference was not statistically significant (p=0.729) (Table 3). This implies that the treatment type does not affect the PIP joint ROM.
To evaluate the functional capacity of the injured finger, we assessed the grip power of the injured hand and compared it to that of the contralateral normal hand. We calculated the percentage of maximum grip power of the injured hand after treatment with the normal side and assessed the level of functional recovery. In the screw fixation group, 50.3% of grip power was recovered at an average of 25.9 weeks follow-up, which was similar to the 53.2% recovery in the K-wire group at an average of 13.3 weeks follow-up (p=0.706) (Table 3).
Contrary to the treatment type, intra-articular surface involvement showed a significant correlation with the PIP joint ROM. In both the screw (p<0.001) and K-wire groups (p<0.001), greater intra-articular surface involvement was associated with smaller PIP joint ROM. This trend was the same across the entire group of patients (including both the screw and K-wire groups) (p<0.001). Intra-articular surface involvement did not have a significant influence on other outcomes (i.e., grip power, time to bone union, and union incidence) (Table 4).
The number of bone fragments did not show a significant relationship with PIP joint ROM in the separate analysis of the screw (p=0.290) and K-wire groups (p=0.110). However, in the entire group analysis, PIP joint ROM decreased significantly as the number of bone fragments increased (p=0.040). Similar to intra-articular surface involvement, the number of bone fragments did not show any correlation with outcomes other than PIP joint ROM (Table 4).
No serious infections, such as osteomyelitis, were observed in either group, although there was one case of pin-site cellulitis in the K-wire group. The K-wire was removed from the patient before the scheduled date to prevent further progression to osteomyelitis. The infection was resolved by intravenous antibiotic treatment during hospitalization. Five patients in the screw fixation group complained of minor dullness at the distal level of the injured digit. None of these five patients experienced difficulties during daily activities and experienced gradual adaptations nearly at the end of their follow-up period.
Intra-articular fractures of the proximal phalangeal head are common, and owing to their structural complexity, they carry the risk of numerous complications other than nonunion or infection. A forward angulation or lateral angulation as small as 5° may interfere with flexion and cause overlapping of the digits. Moreover, finger joints are prone to contractures [6], and therefore, stiffness, deformity (swan neck, Boutonnière), persistent subluxation, and loss of full ROM are common [2,11].
The treatment goal for such fractures is to restore a strong, stable, pain-free joint, thereby achieving optimum ROM and convergence [5,11]. Various treatment methods have been introduced to achieve this; however, few have made direct comparisons between K-wires and screws. While other studies attempted to make a comparison, their patient group was small (n=19) and heterogeneous, including diverse phalangeal fractures, compared to our larger (n=41) and homogenous study limited to proximal phalangeal head fractures [5].
Compared with screw fixation, loss of reduction is more frequently reported in K-wire fixation cases. Moreover, since nonunion increases with displacement [1,6,11], we can assume that screw fixation is better for bone union than K-wire fixation due to the stronger compression force [4]. In contrast, other studies have suggested that soft tissue injury with neurovascular trauma may affect nonunion; hence, screw fixation is inferior to K-wire fixation [1,4,11]. In our study, there was no significant difference in the incidence of bone union between the two groups. Both groups showed a high union incidence in less than 8 weeks, as Barton [12] reported a low nonunion rate of 0.2% to 0.7% in their study.
In terms of ROM, K-wire fixation may be superior to screw fixation because of the reduced scar tissue formation. Conversely, a number of studies have asserted that K-wire is less effective than screw fixation, as screws help to maintain a strong and durable compression force between bone fragments. Therefore, surgeons often prefer screws to K-wire fixation. In this study, no significant difference in the PIP joint ROM was found between screw fixation and K-wire fixation.
Several studies asserted that the percentage of intra-articular surface involvement and the number of bone fragments exert larger clinical implications than the type of fracture [7,13]. This is because the prognosis of articular fractures is influenced by the extent of articular involvement and joint congruity. Therefore, we studied the relationship between the percentage of intra-articular surface involvement and the number of bone fragments with treatment outcomes (i.e., bone union, time for union, PIP joint ROM, and grip power). This investigation was performed in both the screw and K-wire groups, as well as in the entire group of patients (Table 4). As a result, in both the screw and K-wire patient groups, those with greater intra-articular surface involvement had a poorer range of and decreased PIP joint ROM. This trend was also observed in the entire group. Moreover, in the entire group of patients, PIP joint ROM decreased significantly as the number of bone fragments increased. These findings entirely contradict our original hypothesis that there would be a functional difference between treatment modalities (i.e., screw or K-wire fixation). Instead, the functional prognosis of proximal phalangeal head intra-articular fractures may be determined by the percentage of intra-articular surface involved and the number of bone fragments, regardless of the treatment choice.
Pain after proximal phalangeal head intra-articular fractures is common, and nearly 34% of patients may experience pain or cold intolerance [11]. Previous studies have reported that the screw fixation group showed a greater degree of cold intolerance and numbness after surgery [7]. This matches with our study, in which five patients in the screw fixation group complained of numbness, while none in the K-wire group reported this effect. This may be due to stretching or trauma of the digital nerves during screw fixation. However, these data lack validity as we did not administer objective surveys such as DASH (Disabilities of the Arm, Shoulder, and Hand) or visual analogue scale scoring, as in other studies [2]. Instead, we relied on a retrospective chart review, which makes it difficult to assess the level of symptoms or underestimate it.
Rehabilitation of the PIP joint is difficult because of the occurrence of postsurgical subluxation, stiffness, osteoarthritis, and flexion contracture [3]. Currently, there is no consensus on the timing of active and passive mobilization; however, numerous studies have emphasized the importance of early motion [14]. Lengthened immobilization may hinder joint hydrodynamics, which causes degenerative changes and fibrosis in the finger joints. Several studies have revealed that immobilization for longer than 4 weeks may cause stiffness [4]. We applied intrinsic plus-positioned volar protective splinting after surgery [4] and encouraged active and passive ROM as soon as swelling and pain subsided. The time until passive full ROM at physical therapy was 46.7 days for K-wire and 34.5 days for the screw fixation group, and the length of the treatment varied between individual patients [15,16]. The method, length, and timing of joint mobilization varied among patients; hence, we could not draw meaningful conclusions regarding the relationship between early mobilization and PIP joint ROM in our study.
Our study has several limitations. First, the age and the level of injury may have had a significant influence on prognosis, but we failed to consider these two important factors. Second, the grip power was measured on different sides of the hands as we could not measure the grip power of the injured hand in its normal state before trauma. This may have caused serious bias in patients with large differences in the strength of both hands. Finally, K-wires are applicable to small bone fragments, whereas screws are applicable only to patients with large fragments, which are approximately three times larger than screw thread diameter. This blind spot triggered a difference in the indications between the two treatments [4,7].
In proximal phalangeal head intra-articular fractures of the hand, the treatment modality of whether to use a screw or K-wire does not affect treatment outcomes. Instead, as the percentage of intra-articular surface involvement and the number of bone fragments increases, the PIP joint ROM after treatment decreases significantly.
Fig. 1.
An example of the intra-articular surface assessment. The red arrows indicate the width and diameter of the entire articular surface, and the yellow arrows indicate that of the dominant (i.e. the largest) bone fragment.
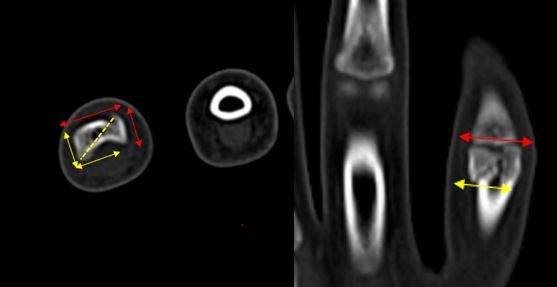
Fig. 2.
Twelve-year-old boy came with a proximal phalanx head fracture by physical fight. (A) Preoperative plain X-ray, computed tomography, and immediate postoperative X-ray follow-up with single-screw fixation. (B) Follow-up images at the 49.7th week, showing return to nearly full range of active proximal interphalangeal joint motion and X-ray showing bone union.

Fig. 3.
Ten-year-old girl came with proximal phalanx head fracture during playing volleyball. (A) Preoperative plain X-ray, computed tomography, and immediate postoperative X-ray follow-up with double Kirschner-wire fixation. (B) Follow-up images at the 15.6th week, showing return to nearly full range of active proximal interphalangeal joint motion and X-ray showing bone union.
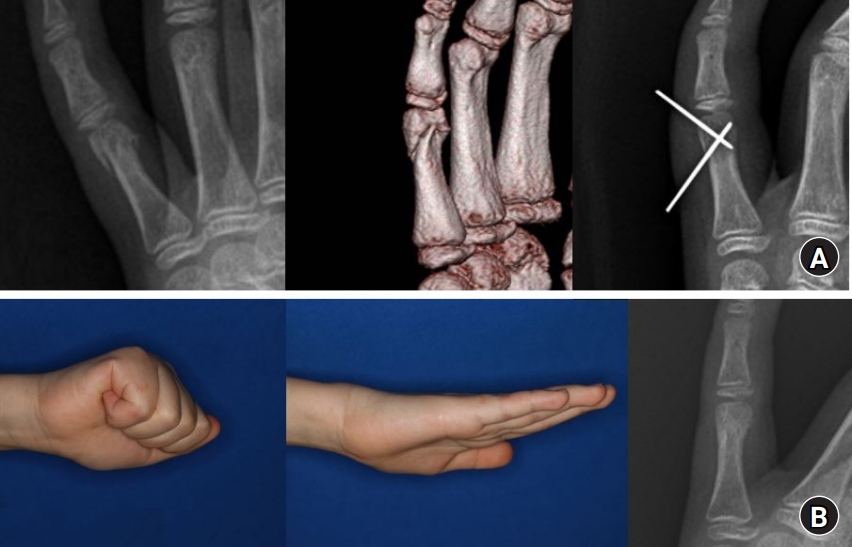
Table 1.
Patients with screw and Kirschner-wire fixation
Table 2.
Comparison of demographics and fracture characteristics between the two fixation groups
Table 3.
Comparison of functional outcomes between the two fixation groups
Table 4.
Relationships of intra-articular surface involvement and bone fragments with functional outcomes
| Functional outcome |
K-Wire group |
Screw group |
Entire group (K-wire+screw) |
|||
|---|---|---|---|---|---|---|
| Intra-articular surface | Bone fragments | Intra-articular surface | Bone fragments | Intra-articular surface | Bone fragments | |
| PIPJ range of motion | –0.878 (<0.001)* | –0.373 (0.11) | –0.861 (<0.001)* | –0.244 (0.29) | –0.881 (<0.001)* | –0.319 (0.04)* |
| Grip power | +0.057 (0.81) | +0.055 (0.51) | –0.367 (0.10) | –0.151 (0.52) | –0.119 (0.46) | +0.019 (0.91) |
| Time to bone union | +0.133 (0.59) | +0.071 (0.78) | +0.234 (0.31) | +0.242 (0.29) | +0.174 (0.28) | +0.155 (0.34) |
| Union incidence | –0.284 (0.22) | –0.285 (0.22) | –0.291 (0.28) | –0.281 (0.31) | –0.203 (0.20) | –0.210 (0.19) |
References
1. Van Oosterom FJ, Brete GJ, Ozdemir C, Hovius SE. Treatment of phalangeal fractures in severely injured hands. J Hand Surg Br. 2001;26:108-11.



2. Borgohain B, Borgohain N, Tittal P. Double parabolic Kirschner-wires as dynamic distractor for treatment of unstable intraarticular phalangeal fractures of hand. Indian J Orthop. 2012;46:680-4.



3. Goldman SB, Amaker RJ, Espinosa RA. James traction splinting for PIP fractures. J Hand Ther. 2008;21:209-15.


4. Freeland AE, Sud V. Unicondylar and bicondylar proximal phalangeal fractures. J Am Soc Surg Hand. 2001;1:14-24.

5. Hamilton SC, Stern PJ, Fassler PR, Kiefhaber TR. Mini-screw fixation for the treatment of proximal interphalangeal joint dorsal fracture-dislocations. J Hand Surg Am. 2006;31:1349-54.


6. James JI. Fractures of the proximal and middle phalanges of the fingers. Acta Orthop Scand. 1962;32:401-12.


7. Aladin A, Davis TR. Dorsal fracture-dislocation of the proximal interphalangeal joint: a comparative study of percutaneous Kirschner wire fixation versus open reduction and internal fixation. J Hand Surg Br. 2005;30:120-8.



9. Minamikawa Y, Horii E, Amadio PC, Cooney WP, Linscheid RL, An KN. Stability and constraint of the proximal interphalangeal joint. J Hand Surg Am. 1993;18:198-204.


10. Jupiter JB, Koniuch MP, Smith RJ. The management of delayed union and nonunion of the metacarpals and phalanges. J Hand Surg Am. 1985;10:457-66.


11. Chinchalkar SJ, Gan BS. Management of proximal interphalangeal joint fractures and dislocations. J Hand Ther. 2003;16:117-28.


13. Chin KR, Jupiter JB. Treatment of triplane fractures of the head of the proximal phalanx. J Hand Surg Am. 1999;24:1263-8.


-
METRICS

-
- 0 Crossref
- 1,683 View
- 44 Download
- Related articles in Arch Hand Microsurg
-
Operative Treatment for Fracture of the Proximal Phalanx Base of the Little Finger1999 ;4(1)