|
 |
- Search
| Arch Hand Microsurg > Volume 27(4); 2022 > Article |
|
Abstract
Vascular malformations of the muscle are rare non-proliferative vascular lesions, and few case reports have described intramuscular vascular malformations in the upper extremities. Vascular malformations of the muscle may produce musculoskeletal deformities due to muscle contracture. Symptomatic intramuscular vascular malformations are commonly treated with surgery and interventional management. We report a vascular malformation that could not be completely resected. It caused adduction contracture of the thumb in the hand. Sclerotherapy was performed before surgery, but the contracture did not improve. Thus, we additionally performed adductor tenotomy. There was no evidence of recurrence during 6 months of follow-up.
Vascular abnormality can be divided into two categories: vascular malformations and vascular tumors [1]. The term “hemangioma” is reserved for true neoplasms, including infantile hemangiomas, congenital hemangiomas, and so on. None of them is normally seen in muscles. Thus, benign intramuscular vascular lesion can be considered a vascular malformation [2]. Vascular malformations are subcategorized according to their flow dynamics as low-flow (venous, lymphatic, capillary, capillary-venous, and capillary-lymphatic-venous) and high-flow malformations (arteriovenous malformations and arteriovenous fistulas) [3]. Such vascular malformations might be apparent clinically as a mass or cause musculoskeletal deformities due to contracture of involved muscles.
Two treatments are commonly performed for symptomatic vascular malformations: surgery and interventional management including sclerotherapy or embolization. Surgical resection is technically challenging due to infiltration of surrounding structures and difficulty in identifying the location and margins of the vascular malformation and bleeding control. Therefore, the choice of these two treatments depends on the size, location, and morphology of the vascular malformation.
We report a vascular malformation occurring in the hand causing adduction contracture of the thumb that could not be completely excised. We treated it with sclerotherapy followed by surgical tenotomy. To the best of our knowledge, vascular malformation causing adduction contracture of the thumb is a very rare lesion that has not been reported previously.
This reports was approved from the Institutional Review Board of College of Medicine, The Catholic University of Korea (No. VC22ZISI0194) and the informed consent was obtained from the patient or the legal guardian for publication of the case report including accompanying images.
A 67-year-old male presented with a right thumb limit of motion that occurred 6 months ago. He had no traumatic event. He had no pain at all and only had a limited range of motion (ROM). On physical examination, active and passive movements of the thumb interphalangeal joint and metacarpophalangeal (MCP) joint flexion showed normal ROM. In contrast, the MCP joint could not extend and the carpometacarpal joint of thumb showed adduction and flexion contracture. There was no palpable mass on hand. He had no pain during ROM (Fig. 1).
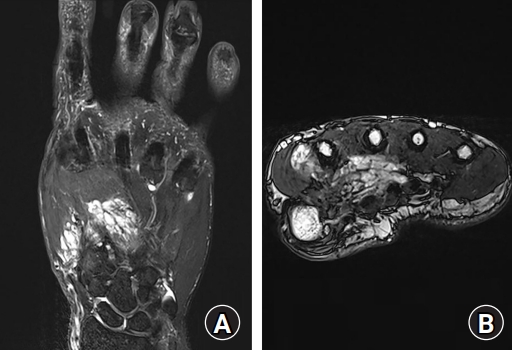
On hand X-rays, a calcific deposit was observed at the 1st web space. The magnetic resonance imaging with enhancement of hand showed lobulated soft tissue mass involving dorsal interosseous muscle at the 1st web, adductor pollicis, opponens pollicis, and palmar interosseous muscle. High signal at T2-weighted image with tubular enhancement suggested intramuscular vascular malformation (Figs. 2, 3).
Complete excision of vascular malformation that invaded adductor pollicis muscle was not possible considering the importance of thumb intrinsic muscle function. Thus, symptomatic treatment was established to gain ROM.
The radiologist revealed that his vascular malformation was a low-flow lesion using ultrasound. Sclerotherapy was performed by an interventional radiologist. After 1 month of motion exercise, ROM was not improved. Thus, surgery was planned.
Volar approach from wrist to thenar crease was done. Possible flexor pollicis longus entrapment and intrinsic muscles were checked. While preserving median nerve and branches, the adductor pollicis muscle was found to be invaded by a vascular malformation lesion (Fig. 4). Transverse head of adductor pollicis muscle belly tightening tension was palpable with thumb abduction. After adductor pollicis tenotomy was done as planned, he gained almost full range of thumb motion. During 6 months of follow-up after surgery, no newly occurred contracture was observed (Fig. 5).
The term “hemangioma” has been used commonly to name vascular tumor and vascular malformation. International Society for the Study of Vascular Anomalies has suggested that vascular abnormality should be classified as vascular tumor and vascular malformation [1]. Hein et al. [2] have reviewed 176 patients with skeletal vascular lesions and suggested that most lesions called hemangioma of skeletal muscle are vascular malformations.
Vascular malformations causing functional limitations have been treated with the whole excision of lesion, sclerotherapy, or both in several institutes [4-7]. The best treatment for vascular malformation has not reached a consensus yet. However, Wieck et al. [4] suggested a management algorism for pediatric intramuscular venous malformations in 2016 [4].
The 5-year local recurrence-free rate has been reported to be 93% after wide and marginal excision, 65% after an intralesional excision without gross tumor remaining, and 33% after an intralesional excision with gross tumor remaining [8].
In the present case, for an unresectable lesion in an adult patient, sclerotherapy was done firstly for a possible gain of ROM to get a smaller size and to decrease bleeding during surgery that might follow. It has been reported that sclerotherapy can be performed for contracture causing lesions to gain ROM in few cases. The present case did not respond to sclerotherapy. Thus, a tenotomy was then performed. As the gross lesion remained, the expected rate of recurrent is high as Bella et al. [8] reported. Ineffectiveness of sclerotherapy might be because repeated attempts of sclerosis were not made. On average, three attempts were tried in the study of Wieck et al. [4]. However, sclerotherapy on contractures seem to be not very effective; in the study of Wieck et al. [4], two of five patient [4] and one of three cases in the study of Domb et al. [7] got contracture relief with sclerotherapy alone.
Surgical management after ineffective sclerotherapy is commonly reported, but mostly, complete resection was done. If complete resection of intramuscular vascular malformations is not possible for reasons such as due to thumb function, the use of sclerotherapy and partial resection or tenotomy could be considered as options for monitoring for recurrence. As a high recurrence rate is expected, adjuvant sclerotherapy could be used. In the case, in concern about the adverse effect of sclerotherapy on new contracture development, sclerotherapy has not been used. In the study of Bella et al. [8], patients were given the options of close observation, re-excision, or adjunctive treatments such as sclerotherapy/chemoembolization.
Preoperative sclerotherapy has an advantage on operation time and blood loss [9]. Postoperative sclerotherapy has been used as adjuvant therapy for incomplete excision as classically. As several adverse effects of sclerotherapy have been reported, clinicians should weigh the pros and cons of pre- or postoperative sclerotherapy to decide in case of incomplete excision in contracture cases.
Fig. 3.
Magnetic resonance imaging T2-weighted fat suppression image. Thenar muscles and adductor pollicis (A), and 1st web space interosseous muscles (B) were invaded by lobular lesion.
References
1. Wassef M, Blei F, Adams D, et al. Vascular anomalies classification: recommendations from the International Society for the Study of Vascular Anomalies. Pediatrics. 2015;136:e203-14.



2. Hein KD, Mulliken JB, Kozakewich HP, Upton J, Burrows PE. Venous malformations of skeletal muscle. Plast Reconstr Surg. 2002;110:1625-35.


3. Flors L, Leiva-Salinas C, Maged IM, et al. MR imaging of soft-tissue vascular malformations: diagnosis, classification, and therapy follow-up. Radiographics. 2011;31:1321-41.


4. Wieck MM, Nowicki D, Schall KA, Zeinati C, Howell LK, Anselmo DM. Management of pediatric intramuscular venous malformations. J Pediatr Surg. 2017;52:598-601.


5. Liu Y, Li R, Liu Z, Wang S, Lu L. Intramuscular hemangioma within the biceps brachii causing the limitations of elbow extension and forearm pronation: a case report. Medicine (Baltimore). 2019;98:e14343.



6. Chen RJ, Vrazas JI, Penington AJ. Surgical management of intramuscular venous malformations. J Pediatr Orthop. 2021;41:e67-73.


7. Domb BG, Khanna AJ, Mitchell SE, Frassica FJ. Toe-walking attributable to venous malformation of the calf muscle. Clin Orthop Relat Res. 2004;(420):225-9.

-
METRICS

-
- 0 Crossref
- 1,076 View
- 30 Download
- Related articles in Arch Hand Microsurg
-
Isolated fracture of the trochlea in humerus - A case report -2006 ;11(3)
Glomus tumor in the volar aspect of the finger - A case report -1997 ;2(1)